Click Here for: Numbing During Tie Release
What Are TOTs? (Tethered Oral Tissues)



Click Here for: Top 10 FAQs About Tongue Ties
Click Here for: Dozens of Tongue Tie Facts…Everything You Ever Wanted to Know
Click Here for: A Step-By-Step Guide To Checking For Tongue/Lip Ties
Click Here for: How to Examine a Baby for Tongue-Tie or Lip-Tie
Click Here for: Kellymom Tongue Tie
Click Here for: Feed the Baby Tongue and Lip Tie
Click Here for: Ties vs. Normal Lip Frenulum
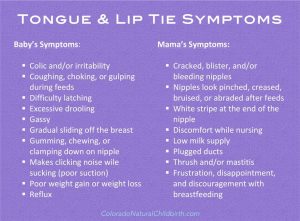
Indicators of Ties
Click Here for: Pain While Nursing
Click Here for: Feeding Issues from Birth
Click Here for: Signs of Distress While Feeding
Click Here for: Not Accepting Solids
Click Here for: Only Eating Purees
Click Here for: Resting Mouth Position
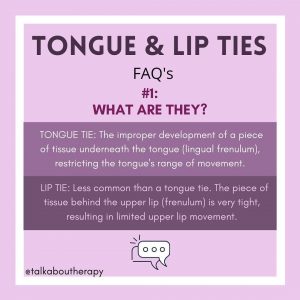
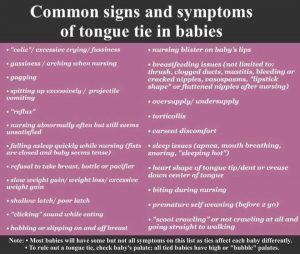
The first sign for ties is difficulty breastfeeding, particularly a painful latch or trouble latching. For bottle-fed babies, you may notice that the upper lip does not flange out on the bottle nipple and/or a clicking noise when Baby sucks. Other symptoms can include bottle/breast refusal, gagging, choking while eating, uncoordinated suck, milk leaking out the corners of the mouth while drinking (seal not complete), slow weight gain, low volume intake, and only eating while sleepy. Some children even display signs of a tongue tie with a heart-shaped tip of the tongue, tongue cupping, or bowl shape of the tongue.
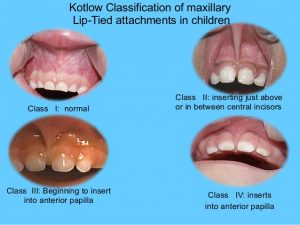
All babies will have a piece of skin between their top two middle teeth and their upper gum/inside of the lip. This does not necessarily indicate a tie. The tie portion of this is, “how restrictive is the skin?” If you pull Baby’s upper lip to the tip of the nose and the skin blanches (turns white), this is a pretty good indication that restriction (exists.
Another huge red flag that your baby should be checked for oral ties is the reason you are likely here…REFLUX! Ties are very frequently found in Gerdlings, as they are one of the root causes for reflux. Baby takes in tons of extra air with these feeding difficulties, and that leads to increased regurgitation as well as painful gassiness, which can also be mistaken for colic.
Other infant conditions that are related to ties are: thrush, plagiocephaly, and torticollis. When there’s restricted tissue (fascia) in the jaw, it can affect really the whole body but especially the neck/shoulder muscles. Typically the tension is worse on one side than the other, so then you get a baby who doesn’t have great range of motion with their neck. Sometimes this + reflux discomfort/Sandifers can lead to torticollis…Fancy word for head always tilting to one side/turning toward one side because of tight neck muscles. It would be kind of like waking up with a crick in your neck—hard to turn it, especially to the “bad” side.
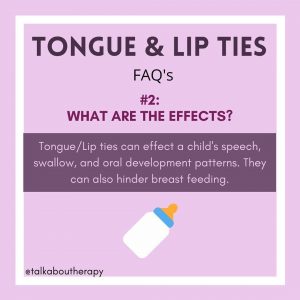
In older children, picky eating, sleeping issues (particularly apnea), swollen/enlarged tonsils/adenoids, mouth breathing, lisps, open-mouth chewing, difficulty starting solids, strong gag reflex, toe walking, stuttering, and crooked teeth.
Jenn H. writes: Often the posterior tie is missed-as in the tongue was not fully released and may still be making it hard for Baby to swallow or move food around to chew it fully. Also posterior ties can keep the tongue from reaching the palate during the swallow and cause extra air to be swallowed. The tongue not resting on palate leads to mouth breathing, especially when sleeping and can irritate the tonsils/adenoids. (But diet can affect that too). Generally, you would only get a tie revised if there are symptoms. And reflux is a symptom of ties. I would also check for a PTT. A majority of lip ties are accompanied by a tongue tie.
Shelley F. writes: A tucked in lip is a good sign of a lip tie as its restricts the flanging ability of the baby. It can be less obvious with bottles as they are usually skinnier and also you can turn by the bottle around the flange the lip. 90% of lip tie babies also have a posterior tongue tie, which is where most of the airtake is and thats what causes a lot more issues.
Stacey M. writes: My ped dentist said hold your mouth open wide as you can and you should be able to touch the roof of your mouth with the tip of your tongue. Or almost touch it. If not, you’re tied. Crazy huh?
Symptoms Potentially Caused by Ties

Jen H., January 2016.
Tongue/Lip Ties and Their Relation to Infant Reflux
When you swallow, the tongue goes up to the palate (that’s what protects the airway when you swallow). When the tongue is tied, it is stuck to the floor of the mouth. It can’t move to the proper position. The result is swallowing extra air. Also for tied babies, it means they have trouble with the typical suck/swallow pattern. Since their tongue has restricted overall movement, they have trouble controlling the flow of milk (breast or bottle), so they choke a lot more in addition to taking in extra air.
Also proper tongue movement stimulates the vagus nerve which lets the rest of the body know that food is coming and to get ready. If that doesn’t happen, then the whole digestive system is off- can be sluggish/cause constipation, etc.
This explains the part about the vagus nerve: The following quote is from here: https://nursingrubysue.wordpress.com/tag/vagus-nerve/
The Vagus nerve…is the nerve that connects the digestive system to the brain. Amazingly, it runs right under the tongue.
This is why tongue-tie is such a problem! The vagus nerve is stimulated to release signal the digestive system to work by the tongue moving. If tongue is tied down by a tight or restrictive frenulum, then the vagus nerve is not stimulated. It never gets the message.
It’s like having mail at the post office that you don’t know is there for you and a mail man that won’t deliver the letters to you. You never get the message.
Your stomach never knows to make acid. So the food doesn’t digest timely. It ferments in the belly and bubbles up into the esophagus causing reflux. Most babies that take reflux medicines just need a tongue-tie revision.
National Institute of Health: Vagus Nerve and the Brain-Gut Axis
Tongue tied babies often have a hard time maintaining their latch (you hear a clicking sound), and when they lose suction they swallow air.
The following quote is from here: Weight Gain is Not the Only Marker of Successful Breastfeeding
Parents can often feel or hear air in their child’s stomach, and burping doesn’t always work to get it out. This air can act as propellant, causing silent reflux, spitting up or even projectile vomiting. The baby can have significant abdominal discomfort as a result.
Stacey M. writes: I don’t want to jinx it but the dentist said she has had cases where the tongue revision DID correct the reflux and no meds were needed after!
Brittney Z. writes: Our preferred provider said the same in regards to reflux symptoms. Said in a study of 1000 babies w ties and reflux 75% saw improvement in reflux symptoms with revision of ties.
Morgan T. writes: We were able to completely stop meds . My baby was vomiting (projectile) every feed and then stopped
Jen H., April 2017.
Advice for Tongue/Lip Ties and Reflux
- Use a preferred provider to make sure that the tongue is completely released
- Get a team in place to help with breastfeeding and recovery of baby (before revision, if possible). Include: a lactation consultant, cranio sacral therapist/ bodyworker who’s experienced with ties, and speech therapist. Here is a List that is specific to finding bodyworkers for tongue tie. Search for Myofasial Therapy in this Directory.
- Be patient, average time for baby to figure out tongue movement and improve on feedings is a couple of weeks to about a month.
- Do bodywork before and after procedure, if possible. I cannot stress the importance of cranio sacral therapy, cst, enough! Find a CST; It is so helpful to have bodywork to release the tensions that the body has from compensating for the ties, or even a quick birth or being malpositioned in utero. How Craniosacral-Therapy Can Improve Breastfeeding. Find if they have experience with resolving torticollis or plagiocephaly; those structural issues seem to be more common in tongue tied babies.
- Unless stitches were used, stretches after a revision are recommended to keep the tie from reattaching or developing scar tissue. Without stretches, it is likely that there is reattachment and the restriction is still present: The Importance of Active Wound Management Following Release from Ties, Frenotomy
- Try nursing in the laid back position, it helps baby control the flow until they get used to everything.
- White noise (loud) can help a distracted/frustrated baby settle down to nurse.
- Make sure to do stretches to prevent reattachment. Luna Lactation has some great videos on YouTube:
- Keep up with pain management for the first week.
Appropriate Treatment of Ties – It Takes A Team

Click Here for: Is Your Baby a Tether-Berg or a Tether-Floe?
Click Here for: Orofacial Myofunctional Therapy – Part 1
Click Here for: Orofacial Myofunctional Therapy – Part 2
Click Here for: The Importance of Active Wound Management Following a Fenotomy
Tongue/Lip Tie (Click here for a List of Preferred Providers!)
The best person to assess and revise for ties is a pediatric dentist with special training in tethered oral tissue. Some SLPs and IBCLCs may have enough knowledge and experience to identify ties as well. A functional assessment for mobility needs to be performed (this means physically/in person). It can be very difficult in most cases to determine whether or not there is in fact a tie by just an image alone.
The best place to look for the most skilled providers in your area is the group for your region found in the link above. Your biggest ally right now is going to be reviews from other parents. This group will likely have information about not only pediatric dentists, but also IBCLCs, CSTs, SLPs, OTs, and other professionals you may need help from to bring Baby’s body to its optimal functioning.
The following people are NOT qualified to rule out ties/tell you they do not need to be treated if they do exist:
- Pediatricians
- Lactation Consultants/Counselors (typically present in hospitals after birth)
- Hospital Doctors/Nurses (even NICU Nurses)
- ENTs
- GIs
- Even some pediatric dentists, if they don’t have the necessary experience and training.
If one of these providers is able to identify the ties, that’s great! However, in our collective experience, they very commonly either miss or downplay them. Even if your baby was identified to have an anterior tongue tie at birth (attached at the tip of the tongue) and it was cut at that time, it is always worth getting a second opinion by a PREFERRED PROVIDER to make sure there isn’t a posterior tie as well.
Sometimes we can tell if a baby needs body work a little or a lot before and as needed after a release. Here is a list of indicators that would give a clue as to whether body work before and after is extremely important. Thank you, Michelle Price Emanuel, manual therapist extraordinaire, for providing this information.
- Jaw clenching
- Decreased jaw movement during sucking
- Chompy movements instead of sucking
- Significant head turning preference to one side/torticollis
- Head flattening/molding/plagiocephaly
- Facial asymmetry
- “Fussy” baby/cries in car seat/cries after feedings
- Arching/extension of spine movements
- GI Symptoms
- Mouth Breathing
- Tense body
There are improved outcomes after a surgical release when body work is done prior to and after a frenotomy.
Karen K. writes: I strongly suggest you find a preferred provider within driving distance (ours was 4 hours away) instead of just trusting any ENT/ped/LC/dentist. Too many false negative diagnoses, incomplete revisions, or just bad advice. I absolutely would not settle for revision in the OR under general anesthesia; it is completely unnecessary and indicates the ENT is not an expert. He is relying on “do symptoms improve” instead of knowing himself how to completely revise the first time–that makes me so mad. And he may not recognize a posterior tie nor know how to deal with it. A preferred provider will revise with laser while baby is awake. It is relatively painless and cauterizes any slight bleeding that may occur. PPs can offer slight calming meds for older children, but I’ve had a 3yo, 2yo, and 13 month old all revised with no meds and they were fine and eating popsicles after.
Lasering is the best option for the LT. If it were TT, you might be able to get away with a scissor clip in the office, as long as you have a way to know there is no posterior TT (cannot scissor a PTT). We had procedures done at 3 days (midwife, scissors), 3 weeks (ENT, scissors), and finally 13 months (PP, laser). The last one changed everything. I strongly regret waiting.
Regarding money, double check with the dentist. Usually they can bill as either medical or dental (usually medical), though I understand your insurance may not indicate them as “in network” if they are a dentist office. They will be the most experienced at finding out how to get it paid. I recognize you may have already tried this. Most will also do a cashpay discount. I had all three of my children revised at once. Because one was on Medicaid (foster-adopt), we had to cash pay, but at a discounted rate, esp. since he needed both LT/TT done.
Jenn H. writes: Seems like it’s common for pediatricians to miss. Some babies just need the revision and are fine, but some babies need a little extra help, working through everything. The body does some weird things to compensate and sometimes those issues don’t just disappear. I also recommend keeping up with pain meds, good aftercare/stretches to prevent reattachment, bodywork and possibly help/therapy from a feeding specialist/speech therapist if needed. Some babies do need some extra therapy/help developing the proper mouth muscles to become fully functional and successful at eating in addition to releasing the ties. Make sure to follow up with CST. (Do before if possible too.)
Revision plus additional therapies resolved all my son’s issues- reflux, gassiness, and feeding aversion. I am pro revision (I actually got mine revised last summer) but I believe that lots of research is needed and additional therapies in order for the revision to be successful.
We jumped into the first revision- we were desperate for a solution. Unfortunately, the revision was incomplete and we didn’t do any aftercare so scar tissue formed and caused more restriction.
The second time we went to a preferred provider, did aftercare, followed up with an ibclc, speech therapist for feeding therapy and lots of cst.
I can’t say enough good things about cst. My son always turned to one side, had pretty bad plagiocephaly, and a lot of tension from his ties. After just the first cst treatment, he was so much more relaxed, able to ride in his car seat without screaming and slept almost the whole night that night.
He was able to nurse better too. After a few treatments, he finally relaxed while nursing, instead of clenching his hands by his ears. Also, he had trouble pooping before cst, something about a tight pelvis, and the adjustments helped him so much. He went from pooping once every 7-8 days to 3-4 times a day.
For many babies, revision is just the first step in a complex process of getting the mouth and tongue to function well. It is unfortunate that there is so little research out there, lots of conflicting info, doctors with little knowledge or a refusal to acknowledge the problem, and parents have to filter through all that crap to help their struggling kiddos.
Older babies may need a little more help- their bodies have been compensating for longer. My son was 4 mos at revision. It was life changing for us. Took about a month for him to eat/ feel great, but he had developed quite an aversion bc of the ties.
I have a friend whose daughter was around 4 yrs old at revision. She gained more weight in the couple of months after revision than she had in the previous year!
Danielle D.B. writes: An ENT did my son’s FIRST revision then since it wasn’t fixed a peds dentist did it properly. I don’t think the title is the important thing. Get as many personal referrals as you can. In our case bodywork was done by a PT but it’s more commonly done by chiropractors. She also did CST. Much like the release I think the process is only as good as the provider and it is unfortunately hard to find someone who is really good at it.
Lindsay T. writes: We’ve been doing CST for four months, and after one visit we saw a difference. Within a week he was nursing completely different and started gaining weight! We go once every week or so. It’s like a massage and he loves it! I couldn’t recommend it more.
Sarah C. writes: My daughter’s ties were missed by all lactation counselors/consultants at the hospital, her pediatrician, and even a private IBCLC that came to our house. [I will put pictures below this blurb.]
She could extend her tongue past her gum line to her bottom lip (BARELY), and that’s all that mattered to any of them. None of these people caught the signs, despite her awful reflux and difficulty breastfeeding. Everyone commented on how small her mouth was from birth onward. At almost a year and a half old, her CST (a true Godsend) took one look at her at our first visit and said, “she doesn’t have a small mouth…Her cheeks and jaw are so tight she can hardly open her lips!”
From birth, she had difficulty sucking, even on a pacifier. We were finger- and syringe-feeding her expressed breast milk, and even that was a task to get her to suck and swallow.
She latched much easier to one breast than the other; it was like she was constantly too stiff on one side to get into a comfortable position. I gave up any attempts at nursing because she clawed at me so hard every time I brought her to breast. With bottles, she made the most awful clicking noises; the worse the clicking, the more she screamed after eating.
Finally we got to a well-known ENT in our state and I was so relieved that he confirmed she had an upper lip tie as well as a posterior tongue tie. However, he was completely in denial about the fact that ties can contribute to reflux. (Even 3 of the 4 GIs we’ve seen have blown off ties impacting reflux.)
The ENT said she had the mildest tongue tie possible, that everyone has some extent of a tongue tie. According to him, revising it would make no difference since I was no longer breastfeeding. He did agree to revise her lip tie since she was making clicking noises on the bottle. I wish, more than anything, I had listened to my gut instead of this guy. We absolutely should have had her tongue revised, and I really regret that her lip was done with a blade instead of a laser. Even though we did all the stretches and followed aftercare instructions, her lip tie grew back, worse than it was before.
She struggled with torticollis and was in Physical Therapy for months because of it. Our next pediatrician was also dismissive of her ties being any significant problem. When she finally began sticking her tongue out, it veered toward one side. He didn’t see an issue.
Trying to start solids is when I knew that something was still very wrong. She couldn’t chew well, and hated having food in her mouth. Her gag reflux was so strong that she projectile vomited when anything thicker than a Stage 1 puree went into her mouth (and she had never been a “spitter;” silent reflux was always her issue).
She is now almost two years old and has been receiving feeding + orofacial myofunctional therapy from a wonderful SLP, as well as cranio sacral therapy from an amazing OT/CST. We drive an hour each way for both of these ladies. When we have her revision done, we will be making a one-way three hour drive across the border to the next state for the best pediatric dentist within driving range.
*Sidenote: we saw a chiropractor too for a while and it did nothing for us. If you find the type of bodywork they provide is beneficial to your baby, that’s great! But from my experience, our CST is a complete miracle-worker in comparison to the regular chiro.
After our crazy journey, here is some advice I wish someone would have given me a year and a half ago (so instead, I will give it to YOU!)
- Unless there is a medical indication NOT to, revise. Always revise. Ties are midline defects; they are NOT supposed to be there!
- Have a team in place before revision! This means that you need to know not only who your provider performing the release will be, but also…who is going to do bodywork (CST or chiro) for you pre- and post-revision? If you are nursing, who is the IBCLC you’ll be following up with to make sure Baby is feeding well, that can help you trouble-shoot if Baby has difficulty feeding after the procedure? If you’re exclusively pumping, take Baby to an IBCLC anyway! You may very well be able to get baby back to breast with this procedure if you have the desire to do so and the right people who can help you!! If you’re formula-feeding, find a SLP you can reach out to with any concerns about how Baby is taking the bottle after the revision. If there’s not one, try an IBCLC…many of them will help bottle-fed babies, too, simply because they love babies and mamas and have a heart for helping.
- The younger you can have the revision done, the better. It will be easier on Baby in terms of healing (and their muscles having less time to compensate/learn the “wrong” way), and it will be way less torture on you to do the stretches required afterward.
- Go to the best preferred provider you can, based on the recommendations in your state’s group. Don’t waste your time and money on anyone else! Yes, EVEN IF it means driving several hours each way!
- Don’t go to an ENT for revision just because of the medical insurance covering it. Yes, a pediatric dentist will probably be expensive. BUT, the thousands of dollars in therapies a year or more down the road will easily overshadow one up-front several hundred dollar revision cost. If money is a concern, see if the dentist can file it with medical insurance for you or if they will accept your HSA/FSA card. Do they offer payment plans? What about a cash payment discount? It never hurts to ask how they will work with you.

This is a screenshot from a video of our CST getting a great stretch/angle of the tongue. It’s impossible to see unless she is upside down and her tongue is being lifted up.

This is the “right” way to check an infant or toddler for ties. If a provider told you your child didn’t have ties, but didn’t check in a position like this, please seek another opinion!

For reference, this is what my daughter’s tongue looks like if she is sitting upright holding her own tongue up. Her tongue looks completely different when she is laying down and her tongue is being held up properly. (Her tongue tie has NOT yet been revised; this is a photo of the same tongue with no changes to it other than positioning.)

I adjusted the settings of this photo so you can really see the webbing of the lip tie. This was previously cut with a blade (scissors or scalpel) and healed back this way.
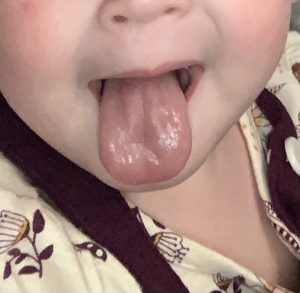
In this picture, notice how her tongue goes toward one side of her mouth much more than the other. You can also see the dimple at the front of her tongue (left side of picture). This is where the tether is attached and pulling her tongue down.
Leaving Ties Untreated
Click Here for: Consequences of Untreated Ties
Click Here for: Connections Between Oral, Airway & Health Problems
Click Here for: Ties are Not a Fad/Trend!
Click Here for: Health/Wellness Podcast Host Discusses Having Her Tongue Tie Revised as an ADULT!
Click Here for: Braces
The effects of tongue and lip ties do not disappear after infancy or even childhood; some of the lasting consequences for older children and adults can be improperly spaced teeth, speech challenges, TMJ, migraines, anxiety, and more.
Julie M. writes: There’s no such thing as a “mild” tie. A tie is a tie and effects the tongue mobility, speech, TMJ and more.
Brooke R. writes: The food gets stuck, and when kids get older etc they can’t use their tongue to clean their teeth, that is if there is a pretty restricted tongue tie present. And with a tongue tie it’s where the tongue lays pressed against the teeth all of the time. I have always had decay and cavities in my top and bottom back teeth. Now I know it’s because of where my tongue has always laid against them. My front teeth I’ve never had any issues with which is why I was confused why it was just my back teeth. Well I know now. I had a lip tie too but when I was 2 I fell and it did tear.
Natalie K. writes: My sister’s son had a tongue tie when he was an infant that didn’t impact breastfeeding and never had it revised…he’s now 7 years old and likely going to have to have it donee. His speech and bite were impacted.
Tanja C. writes: Ties can also cause dental and speech issues and have even been tied to issues beyond that. Like TMJ which I’m certain my ties contributed to.
The effects are not always immediately apparent, but many of us suffer in adulthood from them. A friend recently had hers clipped in adulthood and it has already relieved tension and pains she has had chronically for most of adulthood. Not trying to argue, but just saying there is a lot going on with restrictions that can manifest later and in different ways.
On the topic of age, it is easier to go through with an infant vs toddler, etc. my daughter was revised at 6 months and my son at 4 days. In terms of discomfort, I did not see much difference. In terms of bodywork and recovery time, she did require more. Just my two cents if they help anyone.
Kath R.B. writes: I’m 37 and tied and looking into a revision for myself. So many things I thought were normal and stuff I just had to put up with, well I’m now realising are not and are down to my tie, which I discovered after getting my daughter’s done at 3 months. It was very beneficial for her.
Jenn H. writes: The more I research, the more I am learning how much ties can affect the body-facial development, airway issues, digestion, etc.
I’m all for revising tongue ties (the earlier, the better) bc it affects so many things in the body- facial/airway development, ability to swallow, digestion, body tension, the list goes on.
I had my own tie released a year ago and I am still amazed at how much better I feel in my body.
I saw the preferred provider that I took my kids to. He doesn’t really treat adults, but he did my revision since my kids were his patients.
Symptoms were chronic shoulder and neck tension/issues,(I saw a chiropractor regularly, but my body just didn’t hold proper alignment), frequent headaches, jaw tension, my tongue didn’t rest on palate, couldn’t swallow pills, enlarged tonsils, and sinus issues. I had a lot of muscle tension in my forearms and hips that I didn’t realize I had/didn’t realize was related until after my release.
Also, every morning when I woke up, my body was so tight-I felt like my body had to unwind before I could even move around. I thought it had to do with getting older, but that no longer happens. Also I sleep so much better-more sound sleep, I feel more rested.
Rebekah L writes: In my opinion and in the opinion of my lil dudes pediatric dentist, tongue ties always need to be clipped. They can cause later speech delays depending on the severity. Lip ties if not affecting latch or swallowing of excessive air are mostly seen as cosmetic. That being said, my oldest dude is lip tied and his was never corrected and he’s got a significant gap between his upper teeth. When or if he gets braces he’ll need to have that tie severed to allow his front teeth to come together. My lil dude has his posterior tongue tie clipped and his lip lie left alone. He busted his lip tie himself (and now I see has chipped a front tooth too) and his front teeth have closed on their own. My lil dude had a significant improvement in his reflux issues with his tongue clipping. He also had his clipped at a later age (5 months). It is a relatively easy procedure, recovery is quick, and it was harder for me to watch than him to go through it. There are a lot of reasons to clip lip and tongue tied and very few reasons not too. I personally know speech pathologist that see ties causing speech delays and problems. As far as reflux, my cousin has two children that had one child who had what we consider typical reflux symptoms and was hospitalized twice for failure to thrive. Once his lip was clipped, all his reflux issues resolved. She had the next baby clipped at a few days old and never never experienced any issues.
Posterior Tongue Tie (Nancy C.)
A PTT is a tongue tie but not the typical frontal tie that most physicians and therapist were trained to examine. These were typically the tie that restricted protrusion of the tongue beyond the lip and caused a “sweetheart” appearance. That is normally a stage 1 or 2 tie or ankyloglossia. The posterior tongue tie is essentially a tether of the tongue to the floor of the mouth restricting normal movement of the tongue to collect fluid/food and propel it to the throat to trigger a swallow. The children in an effort to compensate develop an aberrant form of the swallow that cause a slew of difficulties most often associated with aspiration, reflux, “sputtering” of liquids causing coughing choking or gagging. The tether is posterior to the front tie and can only be assessed by feeling for it with the child lying flat and the head in extension on the lap of the examiner.
Two websites of colleagues, that have videos and excellent explanations:
Dr. Larry Kotlow
Dr. Ghareri
I gave you the abridged version, but they are excellent. I am a member of the IATP which provides research & data about this. We see approx 5-8 per week for diagnosis then send to a pediatric dentist for laser revision. We do not recommend surgical cut because the tethers can grow back worse since they cannot “cut” the depth of the tie that the laser can. I hope this helps!!!
Real Experiences from Parents of GERDLINGS
Krista R.
DS had his tongue tie clipped with scissors at birth by our family provider after delivery. He was also a tracheo and laryngomalacia baby. I ended up exclusively pumping while he was in the NICU having a bronchoscopy and he never got the hang of latching, he would scream when offered the breast. He choked on his bottles and we were using the premie dr browns nipples. He ended up having severe reflux and getting an NG tube and G tube for poor oral feeding and weight gain. We found this group and everything got better. At 3 we had him seen by the only Pediatric dentist in our state endorsed by the tongue and lip tie network and they did a laser revision under general anesthesia after lots of months with a medical model speech therapist. He is now 5, the speech therapist that we see specializes in orafacial myofunctional therapy which is what he needs because his tongue does not work separately from his jaw. His speech is ever improving. I regret not having his mouth looked at again by a provider when he was a baby, I think it would have solved so much knowing what I know now and also experiencing the same type of issues with my younger daughter.
DD was my second born and I was hoping to nurse exclusively this time around. My husband and I both heard the awful noises and cried of reflux the very next day after birth. I started doing all of the things and wrote her intro post. When nursing hurt longer then the first week and we had a hard time latching I saw lactation consultants from the hospital with no luck. Instead I posted in a local to me breastfeeding group hoping for a recommendation and one responded to me. She messaged me and said DD must have a tie (even though her doctors and lactation said no). I paid her for a virtual session (she was 2 hours from me) and confirmed. She called the office of the only provider in our state certified with the tongue and lip tie network to get us in within a week. She had her laser revision at 1 month. We struggled afterwards even though she healed nicely and seeing OMT. Our LC gave us extra stretches and I started on domperidone. My supply had tanked due to her inability to transfer milk. This and lots of skin to skin was apart of our reflux journey. We just stopped nursing at a bittersweet 2.5 years old.
Carlie W.
I’m actually a lactation consultant (IBCLC) specialised in ties. When you are taught to correctly assess for issues it becomes easier to see which babies would benefit from revision, which babies can take a watch and wait approach. But you really need to have that discussion with your provider.
Some babies issues are obvious (to me) and causing issues, and I usually recommend release for these babies. Often we discuss watch and wait approach for babies whose parents are hesitant to release, for babies who have an observable restriction but no intrusive symptoms, or babies with complicating health issues. With a lot of my watch and wait patients a lot of these are bottle fed babies because they lack the mother symptoms, pain/damage and issues maintaining supply.
My personal thoughts is that bottle fed babies do benefit greatly from release as it allows their jaw muscles and palates to develop as normally as possible. The muscle development and palate shaping of bottle fed babies can be suboptimal as it doesn’t use the same muscles as breastfeeding, so if a procedure can be tolerated I often recommend it.
Maybe have a chat to a lactation consultant? Seems weird I know if he is bottle fed but they often have great insights into how the babies jaw is moving, how they are coping with flow, how much air they are taking on board.
We are really still in the infancy of understanding ties. I am a recommended provider, and work with 2 other recommended providers here in Australia. We have been analysing data on over 2500 babies and the combination of factors impacting on symptoms and how they present seem infinite.
I’ve seen babies with 100% ties with no intrusive symptoms and I’ve seen babies with 45% ties who are unable to latch.
What we can predict though is that where there is an observable restriction there is almost zero chance of no improvement following revision. These improvements may not always be obvious to the parents, but they are to us. The more drastic the symptoms, usually the more drastic the improvement. Sometimes the parents see no change, but we see a wider gape, a jaw moving more smoothly, more consistently. Less tension in the baby, less effort needed on their behalf. And these are the more subtle changes, not the more obvious ones.
I often have mums come to me with “no problems” who decide to have a revision still, who during the post procedure feed simply repeat over and over, “wow! I didn’t know breastfeeding could feel like this, it feels like Nothing!”
Denise F.B.
Tongue & Lip tie revision saved my youngest! He was FTT, 12 months old but stopped growing around 7 months. He was bottle fed, but barely drank anything. I would have to dream feed 2-3 times/night. Half of the solids he’d try to eat would fall out of his mouth. Old women would look at me weird when I told them he was 11 months+ because he was so tiny. I would set my alarm to wake up 2-3 times/night to dream feed him, and he was days away from a feeding tube–then i learned about tongue/lip tie. We had him revised and as soon as we got home, he sat in his high chair and started shoving food in his mouth and was able to eat it. He also started gaining weight and was back on the growth chart within 1-2 months. He gained 3 pounds in 3 months and was released from having to come in for regular weight checks and I was congratulated by the pediatrician (who originally told me the tongue tie didn’t affect his eating…). AND NO FEEDING TUBE. Call me the crazy tongue tie lady all you want, but it was THE BEST thing we ever did. THe stretches are awful and your baby will cry, but you have to remind yourself you’re doing this for their own good.
They do get sore, and it seemed like days 3-5 were the worst pain-wise, but I’d do it again in a second!
You don’t always have improvement of reflux from a tongue tie revision, if the reflux is caused by an anatomical issue (other than the ties) or from dietary issues. For us, it didn’t fix the reflux, as my son had food intolerances, but it enabled him to drink and eat. He started gaining weight and we avoided a feeding tube. I call that a win!
Hang in there, it will get better!
Caileigh P.
She was born at 28 weeks last mid November. In the hospital after having her have poor transfer at the breast multiple nurses and drs said she didn’t have ties. Her doctor and my doctor said she didn’t have ties. My lactation consultant said she didn’t have ties, her breastfeeding issues were due to my anxiety
Yesterday at 10.5 months old we saw a PREFERRED PROVIDER. Her lip was tied so badly they said left alone her lips may not have closed properly when she got older. Her tongue tie was so bad she barely had any tongue movement and it was no wonder she had so many issues surrounding feeding and they couldn’t believe so many people told us she didn’t have ties. Needless to say both were lasered yesterday. I should have listened to my gut sooner instead of letting others brush us off.
Basically if you’ve been told no your baby doesn’t have ties only listen if it’s a preferred provider. They are the only ones experienced in actually seeing and diagnosing them properly. She’s been home for 8 months now. 8 months ago I had an appointment scheduled and canceled it after being told it would be a waste of my time. Well we drove an hour away and now my girl is already better with her feeding and baby babbles but we have a long way to go to retrain her mouth. Listen to your gut. See a preferred provider!
Before her revision her daily total was like 600mls. Now she hits over 1000mls on a regular basis. Just a month and a half from her revision.
Shirley M.
After revision at 5 weeks old (lip and tongue) by a pediatric dentist, LO was less fussy and squirmy at the breast, not as much arching during feeding, no more clicking noise when nursing, etc. He also stopped being such a noisy sleeper.
The pediatrician pointed out the tongue tie the day he was born, but as a first time mom I was overwhelmed and began researching but saw conflicting things so I didn’t rush to revision. Honestly once I read the connection between reflux and ties, that’s when I felt strongly the need to have them addressed. Wish I had done it sooner.
Post-revision we did speech therapy (really just different suck training exercises) and then chiro, both for about 6 weeks. Definitely saw a difference in gassiness after starting chiro visits!
Some type of therapy after the release is pretty crucial, the babies need help learning how to use their ‘new mouth’
We did just take him for his first dental cleaning at 14 months old, and the dentist said there was some reattachment, but she said that is expected given how restricted he was to start. She didn’t seem too concerned but said she would keep an eye on it. (I pray he doesn’t need another procedure later down the road)
Good to know as a newbie: the stretches you have to do several times a day for weeks after the procedure are not fun, but it gets easier after a few days!
Christine W.
A tale of 2 different babies!
- If you DID get ties revised, what positive impact did you see for your Gerdling? (Can be reflux-related or anything else. Ties affect the entire body, literally).
R- started speaking & eating solid, non-pureed foods within a week of revision
B- stopped choking on bottle feeds & learned proper, suck, swallow, breathe pattern. Never needed feeding or speech therapy.
- How old was your LO when the revision was done?
R- 18 months
B- 3 months
- What type of provider did you see?
Ped dentist who specializes in ties
- Knowing what you know now, what type of provider would you NOT recommend?
ENT or ped dentist not specialized in ties, get it done right the first time
- Were your LO’s ties missed at first? If so, by what type of providers/medical professionals?
R- hospital nurses, multiple peds, IBCLC
- Did you wait until baby was older to have them done? If so, do you wish you had done it sooner?
Oh dear God, YES. Doing the aftercare is much easier on a tiny baby not wiggling away & biting you. No months of increased reflux. No months of stress. No speech & feeding therapy needed.
- Did you seek any type of therapy in addition to the release? (IBCLC, bodywork, chiro, CST, feeding therapy, etc.)
R- speech & feeding therapy, quickly graduated after revision
B- CST bodywork, went from only sidelying on a couch to being able to hold & snuggle while feeding
Rebekah L.
My little dude wasn’t correctly diagnosed and correct til 5 months of age. He would take an hour to eat 4 ounces, there was a clicking noise when he was eating. I wasn’t able to breastfeed effectively and his milk protein allergy was also diagnosed post-breastfeeding which contributed to his reflux issues. I was able to stop thickening his feeds after his was corrected, he could use a pacifier finally (before clipping he couldn’t keep it in), and his reflux improved as well due to FAR LESS gas. There is a ton of literature as to why clipping is vastly important for eating and language development. I took him to two lactation consultants, two pediatricians, an ENT, before he was diagnosed by a pediatric dentist who clipped him. He said he had a 50-70% improvement post clip.
I saw a significant change in my lil dude when he had his tongue tie clipped. He had a posterior tongue tie, which was incredibly difficult to diagnose and a pain in the butt to find someone to treat him (but that’s a different story). It took about 2 weeks to see the total difference but his reflux improved tremendously and so did his disposition and gas troubles. His was clipped with scissors, not a laser but my friend had her sons lasered and it sounded a lot quicker and less painful. We weren’t able to stop meds immediately but I was able to stop thickening. I advise against the methods I thickened with and doing it without an evaluation and recommendation from a SLP. I HIGHLY recommend getting any and all ties clipped. I’m actually taking my newest little dude in for a lip tie evaluation and will advocate for it to be clipped not only for my own comfort (BF hurts so much right now) but also for him.
That being said, we still see that ENT for my lil dudes ears and he was unaware of the correlation of reflux to ties and did more research after he saw my son again. He is the preferred provider in my area for military families having ties revised out of office.
Jenn H.
It was life changing for us. Reflux and gas went away completely. We still had to work thru the aversion but he was finally able to eat enough and sleep. (I was surviving on 4-5 hrs of broken sleep if I was lucky. Sleep deprivation is the worst kind of torture!!)
My son had all the symptoms you listed plus he developed a feeding aversion. He was on a max dosing of Prevacid too, but it didn’t help. Getting the revision is the only thing that made a difference. We did it for my son at 3.5 months. Best decision! The ties made it very difficult for him to latch and nurse. Once the ties were revised and he figured out how to work his new tongue, the reflux resolved and so did his feeding aversion.
It can be a back and forth process in the beginning so just keep that in mind if baby regresses a little. (Especially around weeks 2-3 post. The wound tightens up a bit but if you keep up with the stretches, things loosen up again).
Things won’t be perfect right away. There’s a learning curve for figuring out tongue movement and developing the muscles. It usually takes 2-4 weeks to get all that worked out. (My daughter took a little longer)
I recommend doing some suck training exercises in addition to stretches to develop the right muscles. It may also be very helpful to see an ibclc for some help.
For stretches, it’s important to be quick and precise. Using a headlamp and doing stretches with baby’s feet pointed away from you is super helpful. Also try to make stretches “fun”- be playful, explain what you are doing to baby, make silly faces, etc
Cut down on the gassiness immediately. After about a week we started to wean him off the prevacid. No reflux symptoms and no acid rebound. Took about 3 weeks for him to breastfeed great consistently. I’m so happy we did it. I just wish I had found out sooner-it could’ve saved us so much heartache. I second going to a preferred provider. You don’t wanna have to do it twice. Also look into chiro/cst for after. it may take a little while for baby to figure out new tongue-2-4 weeks. Make sure to do stretches so that scar tissue doesn’t develop and it heals well.
Sleep was the last piece of the puzzle for us. In the beginning our best nights of sleep were on the days we did cst. Once we weaned off the solutabs, sleep got better. (About 3 weeks after revision). My son was super dependent on a pacifier and couldn’t self soothe, so ultimately we had to do sleep training to break the habits/patterns we had established for almost five months. We paid for a sleep plan through the baby sleep site. It was a gradual/gentle approach but things were better within a couple of nights. We were lucky bc naps got better too. It’s been a little over a month and we put him down awake for bedtime and naps. He’s only waking once, occasionally twice for feedings at night and his naps are 1-1.5 hrs.
Just wanted to add- although the revision was successful in terms of breastfeeding/digestion, my son does still have some things we have to address bc of the ties. His palate is very narrow, resulting in a crossbite. It does make it harder for him to eat some foods- mainly veggies and meat (things that require more chewing). He is using a myomunchees daily to build up jaw strength which will hopefully help widen his palate, but if not, he will need a palate expander around age 6. His tongue has a good range of motion but likes to rest in the bottom of his mouth, so some therapy with an orofacial myologist is in his future. (Most won’t treat kids under 3 tho). Right now, he’s in speech therapy, has been for about 5 mos, and he seems just about caught up for his age. He’s almost 2.5.
Brittney Z.
My daughter had some sleep issues that first week after her revision. She was perfectly fine all day & at night she fought sleep and me and would wake very often. I don’t know for certain if it was only related to ties but I figured it was. Dentist said it could be pretty sore for a bit. Not sure why nights are worse though.
Stacey M.
Just wanted to update I found a Ped dentist that does laser revisions – no referral needed! My Lo’s Dr said her lip tie didn’t need fixed and said she didn’t have a tongue tie. We went to the Ped dentist today and she DOES have a posterior tongue tie and upper lip tie! We had both revised today, took literally 5min! She froze her mouth first.
I’m so glad I got another opinion!!!!
Omg it’s 72 hrs post revision and my lo is a disaster She fights sleep and now that she won’t take a pacifier it’s taking 2-3 hrs to get her to sleep. She never had this problem before the revision.. I don’t see how the pain could be that bad since she doesn’t seem upset during the day, she’s smiling and does fine. Night time she is a nightmare !!! She’s completely inconsolable and won’t go to sleep. Maybe she’s overtired? She never had these issues I feel like I’m back to having a newborn baby a week old.
Why won’t she take a pacifier but she will take a bottle?
Brooke R.
On Day 6 Post revisions we saw huge improvements, her reflux was basically gone!!! Each day little by little we would see changes, but then it was like out of no where it was gone. We still continued meds though because they did help.
Shannon K.H.
Hi all. I wanted to write a success post for all of you. At 6 weeks we were desperately looking for help. Desperate is really an understatement. After speaking with some of you we found a preferred provider to check our baby for ties. We found and IBCLC that confirmed she was tongue, lip, and buccal (cheek) tied. I didnt even know buccal ties were a thing. She told us ties are a huge cause of reflux- which I knew from all of you. She referred us to another preferred provider to cut her ties. Before and after the procedure we took her to a pediatric chiropractor who specializes in Craniosacral therapy (CST). This is a very important part in tongue and lip ties as it helps the baby strengthen the muscles in their mouth that they havent been using properly. Our baby was also diagnosed with a milk protein allergy. After trying 7 different formulas (yes it was exhausting and frustrating) we followed the suggestion of trying Alimentum Ready to Feed. After about 2 weeks we started to see improvement. We have since been able to take her off of all reflux medications. Our little lady is now 6 months old and thriving. She is still taking the alimentum rtf, her ties healed and didn’t reattach, and she is off all medications. If you would have told me she would turn out to be the happiest baby I wouldn’t have believed you. If anyone needs help finding preferred providers for ties please let me know. It is sooo important to take them only to a preferred provider. Hang in there Mommas! There is a light at the end of the tunnel. Thank you all for your support, advice and educating me about all of this!
Chelsea P.
It’s been a while since I logged in here but I wanted to let you all know that my sweet little guy is doing better than ever and we can’t thank this group enough for all the helpful advice and support! Per the recommendations made here: we switched to a new pediatrician who is just wonderful, we switched to Alimentum RTF, and saw a pediatric dental specialist who found tongue, lip and cheek ties. After about 3 weeks on the RTF formula and about a week after the laser procedure everything changed. It seemed to us that the lip tie was causing the most issues as well as the powder formula. At 10 weeks old Oakley went from screaming the majority of each day and constant struggles with feedings and gas to no problems at all. His sleep is so much better too. We never ended up needing to try proper dosing because everything cleared up with the other recommended changes. He’s almost 5 months now and is happier than ever!
Karen Y.M.
We got diagnosed and corrected by Dr. Scott Siegel who is an expert in the field. My son did have a weak latch because of his ties and that slowly improved over time. The most dramatic improvement after the correction was his ability to tolerate tummy time without screaming in pain. The procedure is a laser release of the ties and was a solid 2 days of pain for my baby. After that its just mild discomfort with 2 weeks of stretches.
I found that my son benefited greatly from his revision. He refused tummy time. Would flip out…screaming…it was horrible. One week after revision he thrived on his belly and this led to his crawling/sitting upright and in the long run helped his digestion.
Just a heads up…the first 2 days my son (who was just under 4 months at the time) needed tylenol for the pain. It was really rough on him. After the first 2 days though he was much better.
It didn’t help significantly directly with my sons reflux and either did the CST but that is because he has an immature esophageal sphincter…we just have to wait for it to mature. BUT I know tons of parents who saw amazing quick relief after revisions. To me it was worth it functionally for my son though. I feel it indirectly helped him with his reflux by allowing him to progress to an upright position quicker.
Randa C.
We did revision at 2 months I was so worried it would change all sorts of things and cause a lot of pain. After that one dose [of Tylenol] he was completely fine. As soon as his were clipped, his latch was better and he was less gassy. The procedure itself is quick and the sooner you get it addressed the better but don’t be afraid about!
Pediatrician in hospital noticed his tie but said since he was nursing it didn’t need fixed. Pediatrician outside of hospital said “why fix what isn’t broken.” We were in OH and when we got home to KS at 2 months of age the Pediatrician immediately sent us to ENT. ENT said the sooner you fix them the better, much less stressful on an infant than a toddler with speech issues. He had reflux and a very painful latch. Revising by then clipping it didn’t phase him. Although we dosed with Tylenol the rest of the day. His latch immediately changed and as a result he was less gassy which helped some with reflux. ENT was 100% pushing, do not wait to revise any tie!
Simi B.
My baby was diagnosed around 8 weeks by Dr. Shervin Yazdi. I suspected ties due to the symptoms we were experiencing – very frequent feeding, sore nipples, mastitis, milk dribbling, reflux, gas etc. I asked several LCs and our pediatrician and they all said he had no ties. I took him to Dr Yazdi and he immediately diagnosed a severe upper lip tie and a posterior tongue tie. We had it revised and started working with a great lactation consultant. We also followed up his release with craniosacral therapy. It took about 2 months after the procedure for everything to come together and for my son to get the hang of sucking and swallowing properly again but it was worth it.
Lindsey R.
My sons reflux got worse about 4 or 5 days post lip and tongue tie release. It took a couple of weeks to notice a difference and two months to see the real results after stretches and continued light massages. The release can cause lots of extra drool which will flare reflux for some little ones.
Tara S.
I’m not going to lie, it was rough. He screamed during, but it was over in less than 5 mins. Then he latched right away and seemed ok. But that first night he was up, crying most of the night. He slept in my arms from 6-9am! After that it gradually got better. The worst of it was only 2-3 days.
Tara C.
We have had 2 revisions (posterior tongue tie, upper lip tie and upper Buccals) What we did for pain management was alternated Ibuprofen and Tylenol every 3-4 hrs for the first week. We stayed on top of the pain so that she was comfortable. Also, if pain is managed it is easier to move the tongue around more which helps with healing. We also gave Arnica (the pellets mixed with 1-2 tablespoons of water) every 60-90 minutes as needed, frozen breastmilk ice chips, and Hylands teething gel for stretches. Lots of skin to skin and warm baths. The first week is tough! Hang in there though because, I promise it gets better!
Michael N.
Mine was the same. Seemed fine right after the procedure then cried a lot for the next 3 days. She’s more efficient at eating. Before the tongue tie lasered it took 30 to 45 minutes to finish 3.5oz. Now it takes 10 to 15 minutes. We are on day 7 post procedure right now.
Vania R.
My daughter had a lip tie similar to this. I don’t have any pics, but we had hers lasered as well as her tongue tie (which was snipped at birth) at 4 months. It’s made a huge difference with feeding (breastfed), no slapping, scratching, rubbing feet now as I think she was getting a lot of air. Sometimes posterior tongue ties accompany lip ties. I would get it checked if you are worried. My pediatric dentist said they wouldn’t do them on the whim that bubs ‘may’ have speech problems…they can still get them revised later on.
Courtney S.L.
Yes, we had posterior tongue tie, lip tie and buccal ties all done!!! First did tongue and lip because we stretched buccal with OT but with growth spurt they tightened up again and oh boy could I feel it in her cheeks and when she was nursing. And yes they can contribute to reflux, look up aerophagia reflux. Our reflux got a lot better with the revisions!! We still have some reflux but maintain on a very low dose. Tried to get rid of the low dose and was bad so she definitely needs the little she is taking currently. Get all of them done at one time!!
Mindi A.
The tongue tie release was ONE of the pieces of the reflux puzzle. He started on Alimentum RTF about a month before his TT release and started on Prevacid shortly before the release. His main symptoms, screaming and bottle refusal, were gone by 2 weeks post-release. He ate so much cleaner and had way less gas and spit-up. Prevacid was a Godsend for his reflux pain.
Kath R.B.
Revision helped us massively. It didn’t completely cure reflux but it it got rid of gas problems and choking during feeds. And she was dropping percentiles like crazy pre revision but put on a kilo in the month following revision. It’s not a quick fix though. I noticed a significant improvement 1 month post revision and a massive improvement 2 months post. Baby needs time to relearn to use their tongue. If zantac doesn’t work I would definitely say try a ppi. Nexium was like a miracle cure for my daughter.
Allison B.
The first 3 months with a gerdling about killed me. I was the most unhappy person ever! It sucks, plain flat out sucks. Everything (change in formula, meds, etc) takes a minimum of 14 days most of the time before an improvement is shown and then if you have to change again you are screwed! We all understand!!!
We had tongue and lip tie done at 12/14 weeks. The first 24-72 hours were horrible but in our case (and as I suspect in most cases) it did help. I won’t lie, the first 24 hours were pretty bad. He cried a lot but we used Tylenol and after 72 hours he was fine. The preferred provider we went to used a laser. He could tell from the minute he looked at my son’s sucking that he was using way too many facial muscles and not his tongue. He explained that the shape of his head (kinda cone headed but back more than up) What was the result of you say his face and muscles to suck a bottle. He asked if he had to take breaks while eating (which he did) and if he was diagnosed with reflux (yes). It was like he knew my child better than I did!
Our son is 17 months old now and seems to be taking in much less air. You can also see him moving and sticking out his tongue a lot better. Because you’re a little one had the correction so young you may not be able to tell a difference in facial features or tongue movement but I promise you it will be there!!
Another thing I thought of that I wanted to share was that our provider told us the reason a lip tie or a tongue tie will help reflux is because there will be less air in the baby stomach, which will help the force thing of formula or milk back up the esophagus. I think this is true unless you have a baby that doesn’t take in very much air at all. If the baby has reflux is truly from stomach acid and not air then you will need to do correct dosing to see the reflux improve.
Katie W.
We did Tongue and Lip ties at 3 months! Noticed a huge difference but still battle reflux. We are still on a PPI. But he no longer struggles to take the bottle and are currently starting solids! Strongly recommend getting the. Revised if present!
Natalie K.
It didn’t fix my son’s reflux, but changed my life breastfeeding. Don’t regret it a bit.
Karen K.
I had both my bio (breast-fed, GERDling, revised at 13mos) and adopted (bottle-fed, no GERD, revised at 2yo) sons lasered. We did not latch until 3 months old. At the time, I had never met another mom who had gotten baby back to breast after so much time.
Improved bf-ed son’s GERD. Reasoning with bottle-fed son was to avoid future dental problems (he already had the upper tooth gap from lip-tie) and speech therapy.
I also had my 3yo lasered (I have a whole family of ties!). She was a trooper and didn’t bat an eye. Still tells me (now 4yo) that it didn’t bother her at all. They all got popsicles afterward. It is really a very safe procedure.
Biggest benefit is to improve breastfeeding (improved upper lip flanging, able to “grab” more of the breast). If that is going well (or for others, who bottlefeed), you might consider other benefits: helps baby keep a seal while feeding, which decreases air intake (air intake exacerbates reflux). Also, lip tie can cause front teeth to come in with a gap between them. The laser procedure is very quick, accurate, with minimal pain. The laser cauterizes the wound to prevent bleeding, and it also kills bacteria, so risk of wound infection is extremely low. Downsides: reattachment is possible, as with TT lasering. Also, I have heard of some cases–I believe rare–in which the followup care for TT/ULT revision (stretching exercises to prevent reattachment) have led to oral sensory issues/aversions. I do believe if you are as relaxed as possible and do the stretches apart from feedings that the risk is minimized, but, well, full disclosure.
Stacey D.
It will help with reflux, just not overnight. it took about 2 months for my son to be retrained (we did it at 5 mo) to keep that lip from curling back under. if you do any homeopathic chamomile, now is the time to do it before and after the appointment. it was hard to watch the procedure, but definitely worth it. they recommended we pack frozen breast milk ice chips & cold teether toys to help if afterwards he needed to reduce swelling and didn’t want to nurse.
I used organic chamomile tea for both of us & borion squeeze tubes bc hylands has lactose. Something cool will help!!
Corey B.G.
We did laser at 5mo. I was terrified but it was the best decision ever! He refused bottle and breast for 2.5 months. Reflux meds helped with the spit up but he still refused. He didn’t have a lot of the typical reflux symptoms either – was always a great sleeper/happy baby but refused to eat. The only way he would eat is after I rocked him to sleep. I was so relieved when the ties were finally spotted. After revision things slowly improved – took about a month. He’s 7mo now and eats great breast, bottle and now solids. After a month post revision all of his reflux symptoms disappeared too. He’s been off meds since revision as well since the medication made him more miserable from constipation. Good luck, I know how trying things must be! I used to spend the entire day trying to get my guy to eat when it turned out it was physically painful/uncomfortable for him with his severe ties.
Danielle D.B.
By the time I found out my son’s tongue tie was not properly fixed we were bottle feeding. He had been hospitalized for his GERD and was failing to thrive. Alllllllll of it got better post ties. I didn’t know he had a lip tie. But I should have cause it was as you’d described! There are some cause studies I found on line that fixing the upper lip fixed GERD for a couple of babies. My son’s did get better instantly but we never had to increase his dose of meds despite doubling his weight. We dropped 2 the same day he was fixed! At 6 months we are about to start weaning his small dose of omeprazole.
Jordi L.
We had both tongue and lip tie released and we see the chiro and no such luck with the reflux. She’s is gaining weight better and she is overall a much happier baby. Her latch was awful though. We did both at the same time so I can’t say whether the tongue tie made a huge difference or not.
Tamara B.
Yes, my daughter’s supposedly minor posterior tongue tie was revised at 10 weeks. Things improved significantly over a couple of months, together with medication. I have no doubt the tie was at least part of the cause. Over a period of a couple of months things got steadily better with her feeding and consequently her reflux (though she was still medicated until 10 months when we were able to wean her off the meds). Prior to that it had reached the point of only being able to feed her while she was asleep – it had become so stressful for both of us, though she had a good latch and was still putting on weight. After the revision her feeds got much quicker too, I think because suddenly she could use her tongue properly!
Meaghan T.
My son is bottle fed and they did his lip, tongue and bucal, he has some pretty serious ties. The pediatric dentist explained that some of his reflux could be due to swallowing more air because his latch on the bottle is poor.
We’re 3.5 weeks post release and his eating has improved and not as big of burps. He used to have man burps.
Crystal K.
We had improvement immediately but it has been a journey. 11 months later and we still have getting body work done to get the tension away. She also needed another revision 3 months later. Something loosened and it was like instant tie overnight worse than before. We did a lot of bodywork to make sure everything was forward and did the second revision. It looks like more of the tie came forward again but with bodywork nursing isn’t painful and she has good mobility. We won’t do another revision unless it as an effect on speech. She is handling solids very well.
Dannie C.
When born, the pediatrician in the hospital said my son was tongue tied but that she does not clip them. She informed us another pediatrician may come discuss it with us ,but to discuss it in the office with our chosen pediatrician. Our chosen pediatricians feelings were that he was latching so it was not a problem. After relocating, our new pediatrician saw his tongue tie and immediately referred us to an ENT. At this point we were already struggling with reflux for over a month. She wanted the ENT to discuss concerns with us, however her concern was the possibility of helping with reflux and she did not want speech issues in the future. The ENT has been, to this day, the most knowledgeable about reflux! At the time of the appointment we were just over two months old. He said it is best to clip as soon as possible, instead of waiting, because the younger the baby the easier and less traumatic the process. He was very upset that the pediatrician in the hospital did not clip it because he said his tongue tie was one of the tightest he’s seen. I was very concerned with pain for our son, but they numbed him and I dosed him once with advil. It honestly never phased him! Immediately his latch was no longer painful, he burped easier, and was much less gassy overall. I am so thankful we had it done! Note – the younger the revision the better per our ENT and thar most pediatricians cannot correctly diagnose ties!
Hilary K.P.
My son had both and we corrected both to make nursing easier for him. In the end he still had a poor latch. Sadly, correcting his tongue and lip did not help at all with his reflux (moderate/severe). I don’t regret the procedures though, he can actually stick his tongue out now!
Charlie’s Story
My son was diagnosed with silent reflux at 7 weeks. We tried zantac first, then Prevacid solutabs (7.5 mg twice a day). It took a full two weeks to see some improvement in his symptoms. It wasn’t perfect, but he refused less feedings and seemed more comfortable. However, he would only nap if held or carried in the ergo. Night sleep was good- he slept for 6-7 hours, ate, then back to sleep for another 2-3.
After 6 weeks on prevacid, he started refusing feedings again (developed an aversion), was very fussy after feedings, only ate well when half asleep, and nighttime sleep fell apart. He was up every couple of hours all night and would wake at 5am, scream crying and very gassy.
After a lot of research online, I finally figured out that he had a tongue and lip tie. I had a lactation consultant confirm it and the second ENT we saw clipped it. After a week, and only some improvement with feedings/reflux/gassiness, I found out the revision was incomplete. This time, we saw an oral surgeon who revised the tongue and lip with a laser. For some reason- a lot of providers are hesitant to revise the tongue and have a wait and see approach. The thing is, the tongue tie is a midline defect- it’s not supposed to be there and it won’t get better [some believe it’s related to MTHFR]. Sometimes cst or chiro adjustment can provide some temporary relief. It’s so hard to find experienced providers! We had to do the revision twice bc the first ent did an incomplete revision. Oftentimes parents are told to wait regarding the ptt. I just know a lot of mommas that have waited because they were told the tongue wasn’t really an issue and it turned out that it was the main issue.
It took a few sessions with a cranio sacral therapist and a speech therapist to work through all of our issues (Body tension, shallow latch, feeding aversion).
Within a week of the second revision, reflux symptoms and most of the gas issues were gone. Posterior tongue tie (ptt) can cause a lot of issues. When the tongue isn’t functioning properly, it causes baby to swallow extra air, gag and choke, which causes digestive issues. The lip tie also causes extra gassiness because baby can’t get a good seal. With my son, the ptt caused all of that plus, he developed a feeding aversion- it was a lot of work for him to eat and he just got too tired. Also sleep was terrible- he was too uncomfortable to sleep during the day, except in the ergo and every morning around 4/5 am he woke up screaming bc he was so uncomfortable. Post revision (and we did ptt and lip) ALL his issues went away.
Over the course of 3 weeks, post revision, we slowly weaned off the Prevacid solutabs. (We halved the morning dose for a week, then the afternoon, and then just stopped altogether. We needed to give mylanta cherry supreme, mcs, one night, but other than that, there weren’t any acid rebound issues). That made a huge difference with gassiness and scream-crying wake ups at 5am.
By two weeks post revision, he was no longer refusing feedings. At the one month mark, I finally felt like breastfeeding was going normal- he had a great latch and was taking full feedings.
Additional / Related Resources:
Management of Reflux in the First Year
Click here: It’s Not My Milk! Tongue & Lip Tie




