FPIES – Food Protein Induced Enterocolitis Syndrome
Please refer to bottom of the page for further links and information!
Contributed by Becky L., February 2017
FPIES is a non IgE food allergy that affects the gi tract. It is a delayed response rather than an immediate response. FPIES is considered rare and is usually outgrown in phases. For instance, a child may outgrow one trigger at age 3 and another trigger at age 5. It is important to note that there are no tests to confirm FPIES. There are only tests to rule out other conditions.
FPIES is diagnosed by an allergist, gastrointestinal doctor, or a pediatrician. In most instances, an allergist will perform skin prick allergy testing and/or blood allergy testing to rule out IgE food allergies first. Then, after taking a medical history and examining the child, the allergist will diagnose the child with FPIES. Your allergist should give you a letter for ER staff to make them aware of to treat your child in the event of an acute FPIES reaction. It is often the experience of parents that this is where the medical community involvement ends.
As tests can’t confirm what your child will or will not react to before you trial a food, the only way to proceed is to trial foods. This is most often left up to the parents. There are occasions where an in-hospital or in-office trial will be performed. Those are usually left for retrials of known acute triggers or highly likely triggers such as cow’s milk. This brings me to the two recognized types of reactions: acute and chronic. This is where the medical community disagrees slightly, but there is becoming more consensus among most doctors.
If you suspect your child may have FPIES, the first thing you should do is avoid any food you believe may be a trigger. Make an appointment with an allergist. Try to find an allergist knowledgeable in FPIES, as not all are. Next, know that you are your child’s biggest advocate. You know your child best. Keep a food journal. Trigger foods should not be re- trialed for 18 months after a fail. If you are having trouble reaching baseline, a gut rest may be in order. Put baby on breastmilk/formula and only known safe foods for at least 3 months. Then, once baseline is reached, trial new foods.
Two Types of Reactions:
- Acute: This is mostly about timing. There is a characteristic delay of 2-4 hours before onset of severe and repetitive vomiting (parents often report to bile) and eventually diarrhea. The child may appear very ill and sleepy (lethargic), and may become pale or blue. When evaluated by a doctor, he/she may be found to have low blood pressure, seem dehydrated, have a low body temperature, and have blood tests that mimic infection (sepsis); which in some cases can lead to sepsis-like shock. Many infants who are eventually diagnosed with FPIES are initially suspected to have a severe infection or sepsis. When treated with Zofran and iv fluids infants almost always make a fast recovery and this is why they are often thought to have a stomach bug. Many times, parents are sent home over and over from the er with an infant having an acute FPIES reaction being told by er staff that it is “just a tummy bug”.
- Chronic: Chronic FPIES is more difficult to diagnose. The symptoms of chronic FPIES usually begin within 4-24 hours of ingesting the trigger food. It is an ill-defined condition. It is characterized by intermittent vomiting, watery or mucous diarrhea (with or without blood), poor weight gain, and dehydration. Something that I, and other parents have noticed but is not in any literature I have found, is that when the child is reacting to a trigger food often food will be in the stool completely undigested. This could be what leads the child to become underweight and eventually “Failure to Thrive”. Then, when the trigger food is removed, a baseline stool is achieved. Skin reactions, and symptoms of wheezing or difficulty breathing are not representative of either form of FPIES.
Trialling Foods:
There are a few common ways to trial new foods. One thing that all of these ways have in common is that you start off with a very small, about 1 tsp, amount of food, and slowly work your way up. Some parents will trial foods for 3 straight weeks gradually increasing the amount of the food each day until reaching a full serving. Other parents will trail foods on a 3 day on, 5 day off, 7 day on schedule. With this schedule, you would give small amounts of the food, slowly increasing, for 3 days. Then you would not give the food for 5 days. Then reintroduce the food for 7 more days.
The reason for this type of trial is that some children react to foods after a break. Still other parents will do a more rapid trail and will give the food every day for 7 days and if there are no symptoms, call it a pass. The trial method that parents choose really depend on the child. Some children normally react to trigger foods on the first or second exposure. In that instance a more rapid trial would be sufficient. Some children react after a buildup of the food in their system. For those children, you would want the longer, 3-week trial. And for the child who only reacts after the food is not given for a few days then reintroduced, you would want the 3-5-7 method.
The most common trigger foods are milk, soy, rice, and oats. However, any food can be a trigger. For instance, many FPIES children react to sweet potatoes and avocados. Sugar, oils, and spices can also be triggers and must be trialed as well. Don’t assume any food is safe.
Many doctors do not recognize that babies can react to the proteins in mother’s breastmilk. However, moms who have experienced it can tell you that babies most certainly can. For breastfeeding moms, a total elimination diet is extremely important and keeping a food journal is essential. The most common formulas for babies with FPIES are amino acid based formulas or Alimentum ready to feed (if corn is a trigger). Explanations about the various available formulas can be found here.
Other Help:
It is also very important to find a knowledgeable dietician. With the many diet restrictions that FPIES babies and children have, being able to maintain proper nutrition is, at times, very difficult. Often parents find they need to seek the help of a feeding therapist. Children who have been told “no” about foods for so long, are often very resistant when parents try to introduce a new food. Children begin to associate food with pain or “being sick.” Therefore, they become very guarded and do not trust anything new. Sometimes parents can puree a new food and hide it in a safe food for a trial. Then, if the food is determined to be “safe,” introduce it to the child. However, you run the risk of the child refusing the safe food if the new food causes a reaction.
Leaving Your Child with Others:
Keeping your child SAFE is the most important thing you can do, and one of the hardest. If your child attends daycare or stays with a babysitter you will need to take extra time to prepare the staff and train them on how to care for your child. They should know what to look for in a reaction, the steps to take if one occurs, what to do if there is a suspected accidental exposure to a trigger, and that your child must be kept separate from others’ food. All family members and anyone who cares for your child must be knowledgeable in your child’s safe foods, trigger foods, and reactions. Make sure everyone taking care of your child has a copy of your ER letter.
FPIES and Reflux:
Many children with FPIES also have reflux. Reflux is often an additional symptom of a food fail. However, reflux as the only symptom of a fail is not sufficient reason for an FPIES diagnosis. Treating reflux in an FPIES child can take a little more research. This mostly depends on the child’s triggers. If the child is sensitive to corn, the medication will need to be compounded to be corn free. Properly dosing an h2 blocker and a PPI is very important. If reflux is left uncontrolled, you will have trouble determining if a food is a fail or if the symptoms the child is having is still from the uncontrolled reflux. You don’t want the child to be in pain and develop a feeding aversion and refuse food trials. Treating an FPIES child for any illness with medication takes extra planning on the parents’ part. The parent should not rely solely on the medical community to know every ingredient in every medication. BE PREPARED!
My best advice from a fellow FPIES and reflux mom:
* Take a deep breath. It’s a long and exhausting journey. Your baby needs YOU!! You can do this!!
* Don’t depend on the medical community to guide your journey completely. By this I mean, by your child’s advocate.
* Know your child’s symptoms. Every child is different. One child’s symptoms during a reaction may not match another completely.
* Keep a food journal. Log all food you (if breast feeding) and baby eat and any symptoms that baby has that day. This will help you determine potential trigger foods.
* Keep a detailed list of safe and trigger foods for everyone to easily view. You don’t want anyone guessing.
* Write down all symptoms, trigger and safe foods, and questions before any doctor appointments.
* Take safe foods with you to gatherings.
* Educate, Educate, Educate! Everyone who keeps your child should be knowledgeable in FPIES!
* Always trial foods in the morning.
* Avoid cross contamination. You don’t want your child to fail a food due to cross contamination.
* Make your own baby food so that you know exactly what goes into it.
* Cooked foods are best for trials. There are some exceptions of course!
* Even bottled water can be a trigger, so don’t ever assume anything is safe!
* BREATHE!!
Additional Links and Information:
For Breastfeeding Mothers, Diet to Follow (to help w/ suspected FPIES)
What’s all this about Corn in the Formula? (includes a list of other names for corn/corn derivatives)
Corn Free Shopping: Recommended Products
The Food survey success rate here (click web at the bottom to change the view if on a phone)
Defending Joy (helpful Facebook Page!)
Food protein-induced enterocolitis syndrome and allergic proctocolitis
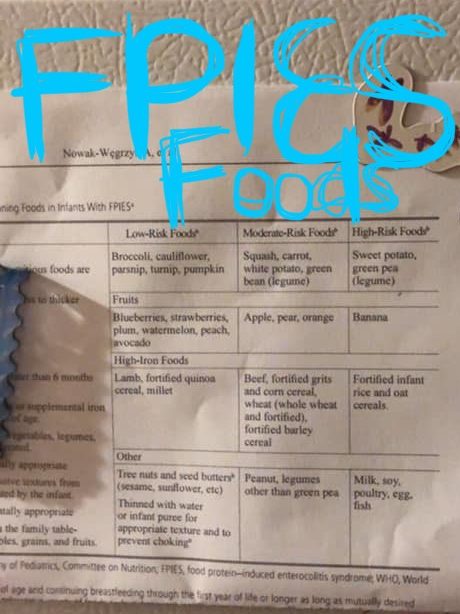
Food Allergy Lists: Classification of Foods