Compiled by: Sarah Camp, January 2021
Contributors: Anke T., Brittney Z., Monica S.D., Becky L., & Sarah C.
The information provided in this article is intended to be used by parents and caregivers of Gerdlings, but anyone may use for informational purposes.
Baby Having Issues Tolerating Solids? Check Out THE Poop Post
Click Here for the link to the Feeding section of the Forum!
Just when you’ve finally gotten a handle on infant reflux and nursing or bottle-feeding, it’s time to start solid foods! This can be a very scary transition for parents of reflux babies. You’ve worked so hard to control the reflux up to this point – the last thing you want to do is throw in something new.
Don’t panic! The key is to just take it slow. Recommendations on amounts, order of introductions, etc. are different from one doctor/organization to the next. Some pediatricians will advise on a schedule for how to introduce solids to your child and which foods they feel are the best.
This article aims to provide some tips that we have found over the years to be helpful for parents with Gerdlings, particularly those who have food sensitivities.
Wait Until Baby’s DIGESTIVE SYSTEM is Ready, Not Just Displaying Other Developmental Signs of Readiness
Anke T. writes: The reason for reflux in many cases is an immature digestive system. So it makes 100% sense to hold off solids for a while longer, until the digestive system has caught up. No matter what official recommendations state, these apply to babies with no health issues.
As a group we support the introduction of solids ɴᴏ ᴇᴀʀʟɪᴇʀ than 6 months. First know that “Food before ONE is just for FUN!” Your baby is not quite ready for solids at 4, 5, and likely not even 6 months of age…not a Gerdling anyway. GERD babies tend to do better with solids in waiting until at least 8-9 months old. KellyMom suggests 6-8 months, but we believe this is appropriate ONLY if & when ʙᴀʙʏ ɪs ʀᴇᴀᴅʏ, ᴘᴏᴏᴘ ɪs ʙᴀsᴇʟɪɴᴇ, & ʀᴇғʟᴜx ɪs ᴡᴇʟʟ ᴄᴏɴᴛʀᴏʟʟᴇᴅ.
Sitting without support, tongue thrust reflex has gone, baby can perform a pincher grasp and bring items to mouth, shows interest in food. *Reaching for food/plate doesn’t necessarily indicate food interest. Baby would take a lipstick tube from your hand and eat it if he saw you do it!*
Reaches & maintains baseline for breastmilk/formula for a minimum of 2-3 weeks before adding solids. Adding solids to an inappropriate milk diet will not only make reflux worse but will make determining food fails more difficult.
We tend to think that a problem with formula or breastmilk poop is a non-issue once solids are added, and that poop will improve with these additions. The problem with this mindset is the assumption that baby won’t still need to have milk once on solids, or even after 12+ months of age. I think we get this perception from doctors and other parents who had non-GERD babies that WERE able to put their babes on cow’s milk or who were able to start solids at 6 months and have no obvious issues. BUT, as much as we hate to say it, our babies are not quote, unquote *NORMAL* in this regard.
And, since most of our babes have to remain on formula or breastmilk past age 1, in order to receive the necessary amino acids for brain development (that alternative milks do not provide), its not feasible to overlook non-baseline formula/breastmilk poops with the assumption baby won’t be on the formula or milk past age 1 and that solids will make poops better.
Do NOT Rush Off of Breastmilk or Formula!
Becky L. writes: Hey wonderful parents. I just want to drop by for a second to give you some hope. I know so many of you worry about switching to an alternative “milk” when babe turns 1. One reason is because you’ve been told your whole life that babies don’t need formula beyond 1 years old. Another reason is because we’ve all been told that baby should be off the bottle before 1. Well let me assure you that this is not necessarily the best advice. If a baby is not on a specialized formula, does not have reflux, does not have food allergies, and is doing perfect with having whole cow’s milk in other foods, then switching to whole milk at 1 years old could be ok. However, if your baby has any of the above issues or any type of problem with food, then it’s ok and in fact wise, to keep baby on formula. With formula often comes a bottle. It’s ok, regardless of what family or anyone else says, to keep baby on a bottle to get the formula down. My daughter was on formula until 4 years old. We’ve had no problems. I know many people who have babies on formula and bottle far passed 1 years old. So, relax, there’s no rush. If baby can’t tolerate cow’s milk then they need the amino acids from the formula for healthy brain development.
Anke T. writes: We need to keep in mind, there are children that just can’t do cows milk; it’s very common unfortunately. And even older children, when diagnosed with milk allergy or even EoE or any EGID are on formula by doctor’s order, some on Neocate even 10 years old and older. As soon as cow’s milk is eliminated the nutrients need to be replaced, and that usually is done with formula.
Sarah C. writes: I just want to add to this, something that has helped ME in my own personal struggle with this issue. My LO is 12 months old & we’ve had a lot of challenges feeding her. Unable to nurse (I knew nothing about reflux, ties, anything at this point), I tried like crazy to EP. Didn’t have that in me, much less an elimination diet with the mental state that I was in. She will probably be on formula until she’s at least 18 months if not longer and that is OK! She’s happy, gaining weight, and meeting developmental milestones.
I’ve spent A LOT of time agonizing over how and what I feed my daughter. But it helps me tremendously when I reframe it and look at it from the point of view as if she *was* breastfed. There is a giant societal double-standard for formula fed vs breast milk babies. Looking at things this way has allowed me to give myself (and my child) so much grace & I hope it may help someone else too:
Formula
- Your baby needs to be OFF of formula by 12 months.
- Everyone is allowed to voice an opinion on bottle feeding (no matter what’s in the bottle) past age 1.
- I wish I didn’t have to warm up my baby’s formula for her to drink it.
Why is my baby so easily distracted from feeling? How come I have to go into a dim, quiet room to feed her? I should just be able to feed her in a crowded place with lots of noises. I must be doing something wrong!
*This is different from aversion/refusal/only eating when asleep.
Breastmilk
- The WHO encourages breast milk until at least 2 years.
- People may have thoughts about a toddler continuing to nurse, but rarely will they voice them especially to the mother as most people understand this is rude.
- If I was nursing, the milk she’d be getting would be warm already.
If my baby was nursing, I would be more likely to withdraw to a calmer atmosphere anyway. I probably wouldn’t be feeding her in a loud, crowded place & even if I did I’d have some type of cover over her.
*The last sentence is just me…I’m extremely shy. If you’re able to nurse in public, I am cheering you on!!
Please know I completely understand that formula and breast milk are two very different things. But maybe the ways we think about them shouldn’t be all that contrary.
Feeding Gerdlings is HARD. Whether you’re on a TED, eliminating a few ingredients (that seem to be in EVERYTHING), can’t breastfeed, decided to give it up because that’s what was best for YOU &/or YOUR BABY, so you’re having to figure out which formula is the best fit……it’s not easy. Let’s not add any more pressure by worrying about what the world around us thinks!
Selecting Foods
Choosing your baby’s first food can be both thrilling and terrifying! Here are some suggestions to take into account:
- We are big fans of meat as a first food for the nutrient density! Beef may not be the best option especially since most Gerdlings are sensitive to dairy. Instead, consider poultry (chicken/turkey) or lamb. You can use the bones and flesh to make meat stock (similar to bone broth).
- Of course, all babies are different in what they will tolerate! However, there are some resources that may offer you a good starting point for choosing foods to trial:
- This is a link for potentially safe foods from a reflux perspective: https://www.infantreflux.org/safe-foods/
- You can also refer to foods from TED diets (posts here and here) for ideas! This applies to both breast- and formula-fed babies. Some ideas are: Grass-fed lamb, Empire brand poultry, Organic/Washed/Peeled/Steamed Pear, Apple, Nectarine, Plum, Papaya, Cantaloupe, Honeydew, *some* watermelon (good for electrolytes, but high in sugar), Blueberries, Avocado, Leafy greens, Bok Choi, Brussel sprouts, Butternut squash, Pumpkin, Zucchini, Yellow squash, Yukon potatoes, Parsnip, Turnip, Rutabaga, Yucca & cassava flour, Chick peas & chickpea flour, Plantains. [Bolded words are ideal starter foods.]
- TED/restricted diets suggests AVOIDING the following: eggs, citrus, tomato/tomato products, rice, wheat, oats, sweet potato, nuts, pea protein, peanut butter, grapes, carrots.
- If your baby has suspected (or confirmed) GI disorders such as EoE or FPIES, you may want to avoid common triggers for those as well.
- Pay attention to food classification/food families! Try to trial one food from each family first. If you notice that Baby fails one food in a family, you may want to avoid that family altogether for a while (definitely true if Baby fails multiple foods in the same family). If you notice that Baby passes a food in one family, you may wish to trial another food from that family in the hopes of an increased chance of success.
- A note about trialing oils (such as olive): make sure to go slow in adding oils to the diet. Too much oil can cause loose stools for any baby, not just those who have an issue digesting something. It’s a normal response to excess oil consumption. By only adding a tiny bit at a time, you won’t have to decipher between a true reaction, or the body just adjusting to the introduction.
- When your baby has known issues with a trigger food, you may need to watch out for more than just *that* word on labels. There are often derivatives of common triggers that like to hide as well. Try to stay away from those as much as possible. Some of the most common that we see being problems/having lots of derivatives are milk, soy, and corn.
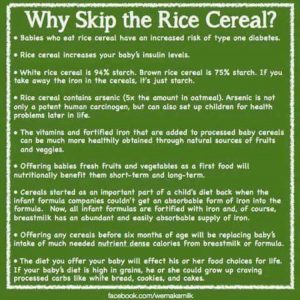
- We strongly suggest staying away from grains (including baby “cereals”) at least when you first begin solids. Grains can be very hard for babies to digest. They do not offer much nutritional benefit, and likely are not worth the risk of “side effects.” For some this is constipation and others simply abdominal pain.
- Check out the excerpt from this article: “until they get their molars—- babies literally do not produce the enzyme in their body that breaks down grains and allows them to be digested. In our families —- that can lead to systemic and gut inflammation.”
- This is another good resource that explains why rice (including rice cereal, rice flour/teething crackers/etc.) should probably be passed on for the time being: Rice Cereal – 4 Reasons To Skip Rice Cereal for Babies
- Why Babies Shouldn’t Eat Grains
- 15 Reasons Not to Feed Rice Cereal (or Any Solids) Too Early
- Eating This Can Tear Holes in Your Gut
- Whenever possible, stay away from canned goods (actual metal cans, not speaking of baby food). These often contain soy and/or corn derivatives. Even if not listed on the label, the cans themselves and inner linings are suspect.
- Potential allergens should be avoided at first as well. When you have a reaction, it can take time for Baby to recover. We aren’t saying to avoid ALL potential (ex: top-8) allergens should be avoided forever, but it is a smart idea to get a good foundation of safe solids before you trial something that is more likely to be a fail. This is because when you do experience a reaction, it’s important to go back to only safe foods until baseline is restored and maintained. When you don’t have any safe solids, or only one to two, that can be really difficult and downright unpleasant for both you the parents and Baby.
How to Prepare Foods
In an ideal world, you’d buy fresh, organic fruits/veggies at the supermarket, and have grass-fed, pastured meats available. If this is doable for you, awesome!
This link has some great info about how to cook and prepare whole foods in case you are interested: Wholesome Homemade Baby Food Recipes: Making Your Own Baby Food Has Never Been So Easy.
However, for those who do not have the time or desire to make their own baby food (or would prefer to be able to at least buy some items pre-made) these are some good guidelines to follow especially as you first get started:
- Start with single ingredient foods, not mixtures of two or more.
- Get organic whenever possible.
- Pouches may be fine, but they should not be used at every meal. This is more about developing good eating skills than it is about the foods themselves.
- Try to avoid things that contain harsh preservatives, particularly citric and ascorbic acid. These are commonly derived from soy or corn, triggers that many Gerdlings struggle with. Even lemon juice may be an issue, but each child’s sensitivity level will differ.
Whenever you have leftovers of your baby’s food, whether it is made from scratch or store-bought, consider freezing instead of refrigerating. Keeping leftovers in the fridge can increase the histamine content, which may trigger reflux. Silicone trays designed specifically for this may be the best thing to store food in in the freezer. Plastics may leech into the food and can cause a reaction if a baby is sensitive to whatever the plastic was made from. Do bear in mind, though, that silicone is also capable of retaining food it has previously held, so it may be wise to discard the container if it was being used to store a food that was eventually failed.
Histamine can also be an issue when you are cooking the foods. Fast methods of cooking (higher temperatures for shorter periods of time) are often preferable over slow-cooked (longer at lower temperatures), which also increases histamines. An example of this would be boiling or baking/roasting chicken (fast) instead of putting it in the crock pot (slow). Instant Pots can be wonderful tools for cooking foods quickly while still maintaining nutritional value.
For uber-sensitive babies, the best cooking tools will be stainless steel and glass. This is because other materials such as non-stick coatings and cast-iron will retain traces of food previously cooked in them. Cross-contamination becomes an issue with those. For some kids, this may not matter a bit, but if you are confused about why your child is reacting to a previously safe food and you’ve used a different tool to prepare, this is something that may be worth investigating.
What About Baby Led Weaning?
BLW is a hot topic right now, and many parents are excited about the idea…for good reason! It allows Baby to be exposed to a wider variety of tastes and textures early on, and prevents having to fix or buy something separate for Baby each time they need to eat. In theory, this sounds wonderful!
There are actually some components of BLW that we agree with:
- Allowing Baby to self-feed
- Offering a variety of textures
- Using BLW guidelines for cutting foods into pieces that will prevent choking
- Eating together as a family at the table
- YOU eating what Baby eats too, so they can see you eating it
HOWEVER, with Gerdlings we need to seriously consider that they are predisposed to having allergies/intolerances/sensitivities, since these were quite likely a factor in why they began having acidic reflux in the first place. These children cannot be expected to eat like a mini-adult. This is where our views with BLW tend to diverge:
- In traditional BLW, the child is supposed to be offered everything the rest of the family has, exactly how it has been prepared (with the exception of being cut differently sometimes for safety reasons). This prevents ONE ingredient from being tried at a time, which is the safest way to ensure that Baby’s entire diet is being fully tolerated. This isn’t just a matter of avoiding cow’s milk and soy, either. Many times there can be a whole host of triggers for GERD, from a seasoning to an oil to the actual “food” (meat, fruit, vegetable, etc.) that you intended to trial.
- Families don’t eat the exact same thing each meal, every day, for 5+ days. This is generally the MINIMUM amount of time suggested to decide if a food is going to be tolerated by a Gerdling. It can be a few days for reactions to manifest due to both delayed reactions and Baby’s “bucket” taking time to “fill” (more on this later). So if you are constantly offering new foods, there is no way to determine which food(s) caused a reaction.
When you have a Gerdling, many things cannot be done “by the book,” and we find that the best thing we can do for our sanity is to just throw the book out the window. A modified version of BLW may work great for your family, as long as you stick to only trying one new food/ingredient at a time, and for the recommended time length. Within that context, by all means offer as many textures as you can and allow Baby to have fun playing learning to feed themselves while enjoying it!
What is the “Right” Way to Trial Foods?
Unfortunately, the answer to this is going to be different for each and every baby. Many pediatricians will tell you to give each new food three days before moving on to the next. They also don’t typically give guidelines for amounts, either. At the end of the day, you are the parent and you know your child best. It will be up to you to determine when your baby is ready for solids, which solids to try, and how much/how long to try them. We can offer some general advice, followed by specific examples for what has worked for some of our families.
Overview
- It is a good idea to trial anything brand new first thing in the morning (and not before nap-time), so that you can observe for any reactions. It is also beneficial for the sake of maybe not being up all night long with a screaming baby if there is some type of reaction that causes Baby discomfort.
- Trial each food for several days/weeks. It can take time for reactions to appear. See our Allergies & Intolerances post for more information. [That post explains the “bucket” that will be mentioned many times throughout the remainder of this article!]
- Less sensitive babies, or those who have pretty immediate reactions, may only need 5-7 days.
- More sensitive babies, or those who have delayed/build-up reactions, may need as long as 10-14 days.
- Start small and work your way up to the amount that you want baby to be eating. This way, if Baby does have a reaction, there hopefully won’t be as much that needs to be cleared out of the system. The more of a trigger in Baby’s body, the stronger the reaction can be, and the longer it will take for Baby to recover to baseline.
- Less sensitive babies may be able to start with one spoonful on the first day, two spoonfuls the next day, three or four the next, etc. until they are at a full serving/jar by the end of the 5-7 day period.
- More sensitive babies should start with a fraction of a spoonful and work their way up even slower. A VERY conservative approach that has been used by some FPIES families in the past is: 1/4 teaspoon on days 1-3, 1/2 teaspoon on days 4-6, 1 teaspoon on days 7-9, and 2 teaspoons on days 10-12. If that’s a pass, the food is deemed safe, and the amounts can be gradually increased to full servings from there.
Least Sensitive Method
- Day 1: one-two bites
- Day 2: three-four bites
- Day 3: five-six bites
- Day 4: seven-eight bites
- Day 5: nine-ten bites
*Some may stop here or at any point after deciding a pass if baby is not very sensitive, or if already at a full serving. - Day 6: eleven-twelve bites
- Day 7: thirteen-fourteen bites
Medium-Sensitive Method
Becky L. writes: The way I trialed was pick a food and make up a few weeks’ worth. Then I trialed that food for a week. I started with 1 teaspoon first day, 1 tablespoon the second day, slowly working up to a full serving by the end of one week. If the food was a pass I picked my second food and cooked it. Then gave it along with the first food. Starting with 1 tsp of the second food with a serving of the first food and so on. I continued adding foods. You can certainly give it a new food alone. If the food was a fail, I waited 2 weeks AFTER getting back to baseline before trialing another food. We did purees for DD for years. Now after a while she had enough safes that some things she liked whole, not pureed.
Highly Sensitive Method
Monica S.D. writes: My kids have delayed reactions so I do a full week for each food item.
- Step 1– Make a list of 5-10 foods you want to trial in order.
- Step 2– Cook the first food and feed it for 3-5 days.
- Step 3– Wait 2-3 days no solids (this is a personal choice).
- Step 4– Determine pass or fail.
- Step 5– Start next food 3-5 days alone (without the previous food)
- Go back to step 2 and repeat.
Once you have 2-4 “safe” foods I fed them those foods for a week or two. Then start over with a new “set” of ingredients. I did a combo of solids and purées. It’s easier to deal with texture and you know how much they eat with purees. You can also do some chunks and some purees of the same food- that was easier for me since I was making my own food.
Our firsts were potato, avocado, banana, chicken and squash (butternut I think). We avoided tomato, peas, carrots, corn and strawberries until they were older. And waited on the “gassy” veggie and fruits (grapes, cauliflower, broccoli) also until they were older too. My kids did eat banana mum mums as toddlers; I introduced those in the second or third set of foods to have something packaged in case of emergency.
Determining Whether a Food Is a Pass or Fail
With a Gerdling, this is more than just a matter of if baby “likes” or “dislikes” a food. It would be great if we could feed our kids everything they enjoyed tasting, but unfortunately that’s not the way it works for them. Instead, our feeding vocabulary consists of words like “safe,” “pass,” “tolerated,” and “failed.”
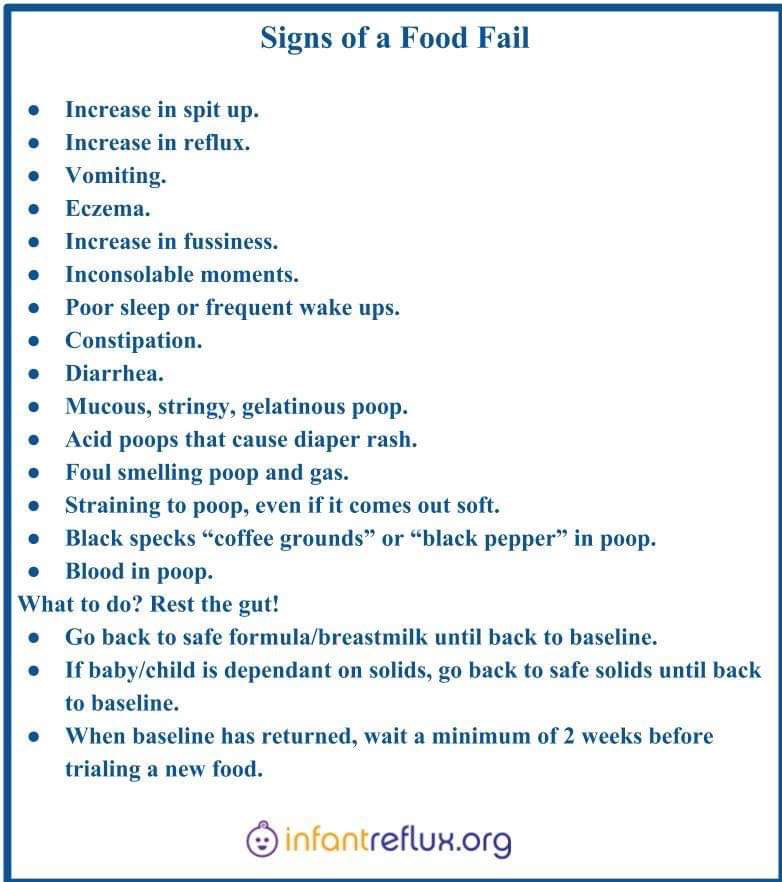
The first and most important thing is to know your symptoms, even the mild ones. Some are more obvious than others, such as screaming, vomiting, and diarrhea. However, constipation, hiccups, short naps, crankiness or bad sleep are precursors of baby being in lots of pain and crying. The earlier you can catch a fail, the faster and easier Baby’s recovery will be.
A food that a child obviously does react to needs to be eliminated. This whole oral exposure therapy (continuing to give the food in the hopes that a reaction will pass) doesn’t work. You can’t desensitize, especially not in an uncontrolled manner by adding it in random form and quantity.
The idea of the body “getting used” to reactive foods is called OIT, Oral Immune Therapy. It intends to expose to a food trigger that a patient has proven allergic to already (either by testing or previous reactions). It’s similar to shot therapy. In its original version it was meant to happen in a doctor’s office each time, with absolute controlled quantities and frequency under the supervision of the provider. It is no longer recommended since all the Eosinophilic Gastrointestinal Disorders came up. And since it never was a good idea to do this therapy as DIY project at home to begin with, the idea does become frightening when you think of the possibility the child has EoE or another EGID already (which never can be fully ruled out in a child with food allergies), so medical providers usually are aware the risk of tissue damage, high eosinophil count and further complications is way too high. That could even be going on for months undetected anywhere in GI tract, so OIT is not a therapy recommended or used for food allergies much anymore.
Gerdlings need to be given the benefit of the doubt when it appears they’re not tolerating a food (reflux increases, poop has mucus or gets firmer, sleep issues develop, etc.). Call the food a fail and give baby a gut rest as opposed to assuming those changes are normal/to be expected when solids are first added, and continuing with trialing more solids. Remember, you can always go back and re-trial a food later if you weren’t totally sure it was a fail. On the other hand, if you assume it’s a pass and start adding new foods on top, that may get you further and further from true baseline. Baby’s “bucket” will continue filling. It’s not the symptoms themselves that cause the allergy/intolerance “bucket” to fill. Rather, the problem foods are filling the “bucket,” and the symptoms are the indications or manifestations of that.
This is what often results in severe reactions developing weeks to months after food has been added making it extremely confusing because you don’t know which food has built up and is now causing the “bucket” to overflow. You won’t know if it’s one food or multiple. This is how reflux gets way out of control once babes get older and begin eating; it’s also often when you see newer symptoms begin to arise–Problems with sleep for example or even ear infections or sinus infections (things brushed off as “normal” for this age, but usually have a root cause).
Anke T. writes: When they don’t sleep at night it’s an indicator they have foods in their diet that are not tolerated and this does give flatulence, stomach pain, but also reflux at a point. It’s a vicious cycle. If a food obviously is not tolerated (sleep alone can show that) there is no sense in “pushing through.” There is no logic behind it. A food will not be tolerated better by more frequent and increase in exposure. A food not tolerated needs to be cut out for quite some time, and can be trialed months down the road again, when the issues are controlled and the child has reached baseline in regards to no symptoms.
Brittney Z. writes: In a month, your little symptoms here and there might become consistent problems as time goes on (snowball effect). The continual exposure to something that isn’t 100% appropriate builds & builds. My daughter had this happen just before her 2nd bday. We were what we thought was corn free/light. Alimentum RTF & reading labels for obvious corn (corn syrup, corn starch, etc) but not so much for corn derivatives. Her poop got more formed & firm but it was daily & what we saw as her baseline (just harder & patty like). We went with the “she’s pooping daily so it’s probably ok”. Within several months of this & adding about 35+ foods (some trialed properly but some not so much) I noticed she began waking some at night, she would gulp & slightly arch but I really didn’t see any pain. I thought she was doing it for attention. Then she started saying “hot” when offered food. Still I missed it. 2 months before her bday she ate a bunch of foods ay my parents’ house that she shouldn’t have. Dairy etc. This led to diarrhea & then vomiting that lasted 2 weeks. We had to back way off solids because we had no idea which food was the issue. It wasn’t just what she had at my folks. It was something that caused her “bucket” so to speak to overflow (resulting in the reaction we saw). By backing off solids and allowing for a gut rest & only offering a few foods we KNEW were safe (because we had trialed them properly), this allowed her bucket to empty of those proteins & is what allowed us to get back to her Alimentum baseline. But it took more than a month for that to happen & once at baseline we worked to add back solids… In doing so we learned that rice, a food we initially called “safe”, actually was not being tolerated. This wasn’t surprising considering corn was already an issue & we later determined wheat wasn’t a great fit. So it was like “grains” in general were problematic for her.
What to Do After a Fail
First thing’s first: go back to only known safes! This may mean only formula or breastmilk. For younger babies (especially under a year), a liquid diet is preferable anyway for this process because it is much easier to digest. For older babies/toddlers, this may mean going back to only known safe foods along with the breastmilk or formula. The fewer foods in the mix right now though, the better. We call this “gut rest.” It is giving Baby the chance to get back to baseline. Allow the body time to flush out the trigger food, reset, and recover.
In the meantime while you are waiting to reobtain baseline, there are some things you can do to help Baby. Symptom control is of the utmost importance! Read more about getting through a reflux flare-up from a food fail here: Fighting the Flare. You can also assist Baby’s body in the detox process through mineral balancing. Epsom Salt baths in particular are great for this. Our Magnesium for the Littles page has explanations.
Once Baby is back to a happy baseline, PAUSE! A good rule of thumb is to wait for two weeks of Baby being fully at baseline before attempting to introduce a new food. This prevents the body from “automatically” reacting to something new being introduced because it’s still in “Fight or Flight” mode from the previous reaction. It also gives you, the parent, the ability to re-learn what your child’s baseline truly is, so you have a good sense of issues when they may arise again.
Don’t I Risk *CAUSING* Allergies If I Delay Solids or Avoid Common Allergens?
There are theories floating around which state that children need to be exposed to certain high-risk allergens (such as peanuts) within a certain time frame to prevent the child developing potentially life-threatening allergies. In kids with normal, healthily developing immune systems, this may be a reasonable and even prudent thing to do. However, we must take into account that with preexisting allergies and/or intolerances, you may be inviting trouble/increasing the risk of a reaction by doing so.
Anke T. writes: It’s not a scientific fact, it’s an assumption. But if that would be true, why does Germany for example have the lowest rate in peanut allergies? Peanuts are not part of diet here, for most adults, and definitely not for infants or toddlers because Germans just don’t eat them much. But still, in some treats like Snickers or things like that, they are an ingredient, and almost every child starts eating those around age 4 or 5 with no problems whatsoever. They would all be ANA if that hypothesis were true.
I Feel Bad for My Gerdling that s/he Isn’t Eating Much Yet or Can’t Have What We Do…
Anke T. writes: It’s good that your baby wants to eat, but saying “no” to foods that you eat is your *duty*, in regards to parenting, when obviously it’s not good for your baby. Children want to do things all the time that parents need so say “no” to; it’s in the nature of things. You can not afford to feel bad about it, but rather get used to it, as this will be most difficult part of your parenting job for the next years to come in many aspects of life. It’s not the end of the world if a one-year-old doesn’t tolerate all of the same foods another one-year-old maybe would. I wouldn’t see it as lack of progress when you cut it all back. Accept the fact that your baby’s GI system is sensitive and s/he needs a basic, and controlled, age-appropriate diet. Your baby will have the rest of her/his life to eat what others eat.
Monica S.D. writes: [If not much food actually gets consumed] Keep offering; remember that playing, touching and mouthing the food counts as a food exposure (for behavior, not allergies). It’s ok if she only has 4-5 things she likes and eats all the time as long as they are safe. My oldest didn’t have safe foods until she was 2.5 and my youngest had safe foods but wouldn’t eat food until she was 16 months. They both eat everything at 9 years and 22 months, except allergens…and sometimes those too when I’m not looking.
Sarah C. writes: It’s so tough with them wanting your food, especially when they can start expressing that or “complaining” about not getting it. My LO is still on a very restricted diet due to ongoing GI issues. I hid from her to eat for a very long time. Or ate while she was asleep. Now that she has a few safe foods, she gets to eat her foods at the table with me while I eat my food. She still wants what I have, but at this point it’s clear that she may be dealing with her allergies/intolerances for a long time, so I’ve gotten in the habit of saying: “This is mommy’s food. You have your food. Mommy eats her food, and you eat your food. We eat together, but we can’t share or mine would hurt your tummy.” My husband and I still eat dinner after she goes to bed. I’m not going to lie, it’s hard. I have cried & agonized over eating & poop more than I ever thought possible.
I feel like a jerk when she wants my food. But on the flip side, some of our family members were watching her a little over a month ago and “felt bad” for her because she wanted their food, so they gave it to her. Not just a little either. She STILL has not gotten over the reaction it caused. It’s BETTER, but she is not back to her old self/baseline with eating, sleeping etc. So when I feel bad for not feeding her what I have, I just have to remind myself that it’s for her own good & being a parent is hard sometimes — harder for some than others, for reasons like these.
Additional Resources
- This is from the Journal of the American Academy of Pediatrics, about breastfeeding. It mentions starting solids.
- This article (click here) states, as we believe, there is no reason to start foods in any particular order.
- Things to Consider When Starting Solids from a Speech Language Pathologist
- SLP Thoughts on Birth-12 Months Feeding
- What Parents Need to Know Feeding Their 12-24 Month Old by an SLP
- This is the baby-led weaning site. ‘Weaning’ here means introducing solids; it’s the European usage of the word weaning (as opposed to the American meaning of stopping breastfeeding all-together, or the InfantRelfux.org meaning of getting off medication)
- Baby Nutrition: Purees vs. Baby-Led Weaning
- Starting Solids, from KellyMom
- FAQ about Starting Solids, from AskDrSears
- Feeding and Swallowing Disorders (Dysphagia) In Children
- Baby-Led Weaning: The Essential Guide to Introducing Solid Foods and Helping Your Baby to Grow Up a Happy and Confident Eater
(Paperback) By (author) Gill Rapley
- Supplement Protocol for Babies Eating Solids
NOTE: The information on this page
is not exhaustive and complete accuracy is not guaranteed. Please
consult your doctor with any questions you may have regarding the
treatment of your child.