Food Allergies and Testing
Anke Tillman, July 2018
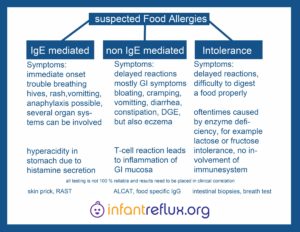
First of all we need to be aware that there are several types of food allergies that may cause reflux and other symptoms in infants. A food allergy is caused by the immune system, it is the body’s response to a food allergen. This is caused by immunoglobulins (antibodies). So far conventional medicine only provides testing for food allergies that are caused by Immunoglobulin E (IgE).
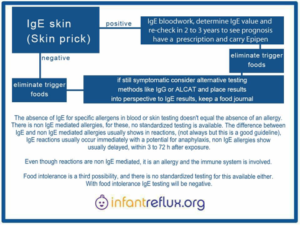
IgE food allergies (Type I) present with immediate symptoms. In between minutes of ingesting the food allergen there will be trouble breathing, hives, redness of the skin, and/or vomiting, all the way to (possible) anaphylaxis. A reaction may affect one or even more organ systems. Testing for IgE mediated allergies will usually start off with the skin prick test. This is a test where very small amounts of the allergens are applied into the superficial layer of the skin. It can take up to 20 minutes to verify whether a local skin reaction is shown or not, and the test will be read at this time. If there are positives, this needs to be followed by a blood test for food specific antigens, (RAST), and this will show the exact numbers of immuno-globulins towards the specific antigen (IgE level in kU/L). The results of this test needs to be kept for the record and should be repeated one or two years later, to see how the numbers have changed. Just because there may be some positives, this does not equal the child being allergic to these foods. It basically means there is potential for reactions towards these foods; the higher the numbers are, the more likely it is to see an anaphylactic reaction. Patients may be sensitized, and therefore test “positive,” but may not be clinically allergic. An oral food challenge may determine, if there truly are reactions. It is not recommended to eliminate all positives if they don´t cause symptoms, as it will reduce the amount of variety of nutrients provided and may increase the risk to get more sensitized and even develop an allergy towards this antigen. If there are positives, and it is uncertain if these are causing symptoms, it is a mandatory precaution to get a prescription for emergency medication such as Epi-Pen and steroid suppositories. The IgE blood levels will change, they will not remain the same over time, as long as the child is growing and developing his or her immune system; they will not be the same for years to come. There is a good chance that these numbers will be outgrown. Most allergists recommend to remove positives (when there are symptoms), then re-test in one or two year intervals, and, if the numbers have decreased, they will order an in-office oral food challenge, so the food may be safely reintroduced.
Another type of food allergies is non IgE mediated food allergies (Type IV). These present with delayed reactions and mostly manifest with inflammation in (gastrointestinal) tissue. It may take up to 72 hours after consumption of the food for symptoms to be observed. Symptoms can vary widely. Some examples: stomach pain, gas, cramping, eczema, delayed gastric emptying, diarrhea and/or constipation. Nasal congestion with no upper respiratory infection and allergic rhinitis are strong indicators for this type of allergy too. As the name already tells, these allergies will not show in IgE testing, neither skin nor blood. There is no test for this type of food allergy. Non IgE mediated allergies are caused by non-IgE antibodies and/or a cellular immune res-ponses (T-lymphocytes). They are also a component (mostly in combination with IgE mediated allergies, sometimes isolated) of disorders such as eosinophilic esophagitis (EoE), allergic procto-colitis and food protein-induced enterocolitis syndrome (FPIES). As for parents of children with these disorders, or patients themselves, it is oftentimes hard to identify what their trigger foods are; recently more and more have reached out to alternative testing methods like IgG testing, ALCAT, MRT, or food antigen specific LTT. These may deliver conclusions in regards to identifying allergens to eliminate, especially in combination with food journals. Even though helpful for many, these testing methods are not standardized and acknowledged by conventional medicine.
There is a third possibility left if a child doesn’t tolerate a food well. That would be an intolerance. An intolerance should not be confused with non IgE mediated allergies, since an intolerance differs by the immune system not having any role in it. It is basically what it is, the child does not tolerate a food well. There is no testing method for this available, only empirical methods of data collection may provide relief, like keeping a food journal.
While food specific IgG testing methods may often help patients to ascertain triggers for their non IgE mediated allergies, the type of allergy they have is not “IgG allergy”. In non IgE mediated allergies, IgG may play a role, for example as it is indicated that IgG4-associated antibodies have a part in EoE. But, mostly, it is T-cell reactions in the tissue, mostly mucosa, that are responsible for the allergic process. Conventional medicine, currently to this day, is convinced that IgG does not play any role in food allergies. So using the term “IgG allergy” is technically not correct. However, there is a great deal of confusion out there, since a lot of providers mix up non IgE mediated with intolerance. So, keeping on track with termoinology can be quite a real challenge.
Non IgE mediated has, up until now, been seen as/thought of as/referred to as ‘IgG reactions,’ however, in diagnosing allergies, hypersensitivities or intolerances, there is no direct involvement of IgG. The only way IgG are related to the subject is that a food specific test may show positive IgG for the allergens in a non IgE allergy (there is no test for this). ALCAT/MRT does test for some specific IgG but also tests for inflammatory markers as well. An intolerance is always something where the immune system (and therefore antibodies) are not involved. So since there is no test for non IgE mediated allergies, one may look to see if IgG tests will give conclusions, but IgG are not part of the allergic process. No one knows why these tests sometimes point out the trigger.
Anaphylaxis in the 21st century: phenotypes, endotypes, and biomarkers
Become familiar with the various manifestations of anaphylaxis, including GI – diarrhea and vomiting, and neurological manifestations such as a sense of impending doom and seizure. Anaphylaxis does not always mean airway closure. Many doctors, including some ER physicians, are unaware of this, so be prepared to advocate for your child.
Anaphylaxis and Atypical Anaphylaxis review from American College of Osteopathic Pediatricians.